When you’re nursing a baby and managing asthma or COPD, every medication decision feels heavy. You’re not just thinking about yourself-you’re thinking about your child. That’s why so many new moms ask: salbutamol and breastfeeding-is it safe? The short answer is yes. But there’s more to it than just a yes or no.
How salbutamol works in your body
Salbutamol, also known as albuterol, is a short-acting beta-2 agonist. It relaxes the muscles around your airways, making it easier to breathe. Most people use it through an inhaler-like Ventolin or Salamol-during an asthma attack or before exercise. Only a tiny fraction of the drug enters your bloodstream, and even less makes it into breast milk.
Studies show that after using a standard puff (100-200 mcg) from an inhaler, less than 0.1% of the dose appears in breast milk. That’s about 10 to 20 micrograms per day, which is far below the amount used to treat premature babies for breathing problems. In fact, neonatal intensive care units sometimes give salbutamol to preemies via IV to help with lung development. So if your baby is getting more than that in the NICU, your milk’s tiny amount isn’t a threat.
What the research says
A 2021 review published in the Journal of Allergy and Clinical Immunology analyzed data from over 500 breastfeeding mothers using inhaled salbutamol. No increase in infant side effects-like fast heartbeat, jitteriness, or feeding issues-was found compared to mothers not using the drug. The same study noted that even mothers using higher doses (up to 1,200 mcg per day) showed no clinically significant transfer to milk.
Another study from the UK’s National Health Service tracked 87 nursing mothers who used salbutamol regularly. Their babies’ heart rates, oxygen levels, and feeding patterns were monitored for six weeks. Results? No adverse events. One baby had slightly fussier behavior, but it was linked to teething, not medication.
The American Academy of Pediatrics classifies salbutamol as “usually compatible with breastfeeding.” The LactMed database from the U.S. National Library of Medicine, which is trusted by obstetricians and pediatricians, gives it the lowest risk rating: L1 (safest category).
How to minimize exposure
Even though the risk is low, you can make it even lower. Here’s how:
- Use your inhaler right after breastfeeding, not before. This gives your body time to clear most of the drug before the next feed.
- Rinse your mouth with water after each puff. This reduces any leftover drug that could accidentally get into your baby’s mouth during skin-to-skin contact.
- Use a spacer device. It helps deliver more medication to your lungs and less to your throat, cutting down on systemic absorption.
- Don’t double-dose unless your doctor says so. More puffs don’t mean better control-they just increase your own risk of side effects like shaky hands or a racing heart.

What to watch for in your baby
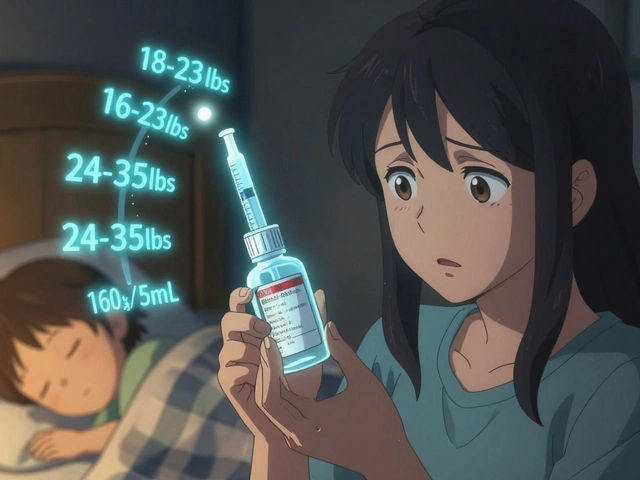
While serious reactions are extremely rare, it’s smart to keep an eye out. If your baby suddenly becomes unusually fussy, has a faster-than-normal heartbeat (more than 160 beats per minute at rest), or refuses to feed for no clear reason, talk to your pediatrician. These signs are uncommon, but if they happen, they could point to a sensitivity.
Most babies show zero reaction. In fact, many moms report their babies sleep better after they use their inhaler-because the mom is calmer and breathing easier. That’s not the drug affecting the baby. It’s you feeling better, which makes feeding smoother and more relaxed.
What about oral or IV salbutamol?
If you’re on tablets or an IV drip-usually only in severe asthma flare-ups or hospital settings-things change. Oral salbutamol gets into your bloodstream more fully. A single 4 mg tablet can raise milk levels enough to potentially cause mild side effects in a newborn, like a faster heartbeat or irritability.
In those cases, your doctor might recommend temporarily pumping and discarding milk for 4-6 hours after a dose. But even then, the risk is still low. Most hospitals allow breastfeeding to continue with monitoring, especially if the baby is full-term and healthy.
Alternatives to consider
Salbutamol is the go-to for quick relief, but if you’re still worried, there are other options. Long-acting inhalers like formoterol or budesonide (an inhaled steroid) are also considered safe during breastfeeding. Some moms switch to combination inhalers (like Symbicort) for better day-to-day control.
But here’s the thing: switching medications isn’t always better. If salbutamol works for you, there’s no need to change. Uncontrolled asthma is far riskier for both you and your baby than the tiny amount of salbutamol in your milk. Poor oxygen levels in mom = less oxygen for baby. Stress and sleepless nights from wheezing? That affects milk supply more than any medication.
Real-life stories from nursing moms
One mum in Brisbane, Sarah, started using salbutamol again after her second baby was born. She’d stopped during pregnancy out of fear. Within days, she was wheezing at night, couldn’t sleep, and her milk supply dropped. After talking to her midwife, she restarted her inhaler. Within a week, her breathing improved, her baby fed better, and her supply bounced back.
Another mom, Lisa, from Melbourne, used her inhaler every morning before feeding. Her baby, now 18 months old, had no issues. She says: “I thought I was being reckless. Turns out, I was being reckless by not using it.”
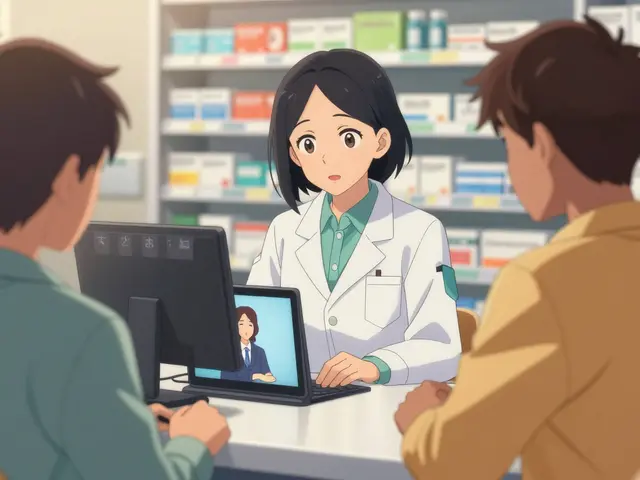
When to talk to your doctor
You don’t need to wait for problems to speak up. If you’re pregnant or breastfeeding and have asthma, make sure your doctor knows. Ask for a review of your asthma action plan. Many moms don’t realize their inhaler dose might need adjusting after birth-hormones change, and your lungs might need more or less support.
Also, if you’re using other asthma meds alongside salbutamol-like steroids or anticholinergics-ask about their safety too. Some combinations are fine. Others need monitoring.
Bottom line
Salbutamol is safe to use while breastfeeding. The amount that gets into your milk is tiny. The benefits of keeping your asthma under control far outweigh any theoretical risk. Your baby needs a healthy, breathing, rested mom more than they need a perfectly medication-free breastmilk.
Use your inhaler as prescribed. Rinse your mouth. Use a spacer. Monitor your baby for rare signs like unusual fussiness or fast heartbeat. And don’t let fear silence your inhaler. You’re not putting your baby at risk-you’re protecting them by taking care of yourself.
Can I use salbutamol right before breastfeeding?
Yes, but it’s better to use it right after feeding. This gives your body time to clear most of the drug before the next breastfeed. Even if you use it before, the amount in your milk is still very low and unlikely to cause harm.
Does salbutamol affect milk supply?
No, salbutamol doesn’t reduce milk supply. In fact, uncontrolled asthma can lower supply by causing stress and poor sleep. By keeping your breathing stable, you’re more likely to maintain a healthy milk supply.
Can my baby get asthma from my salbutamol use?
No. Salbutamol doesn’t cause asthma in babies. Genetics and environmental factors like smoke exposure or air pollution play a bigger role. In fact, managing your asthma well reduces your baby’s risk of asthma by lowering their exposure to secondhand triggers like wheezing and coughing.
What if my baby is premature or has health issues?
Even premature babies can safely breastfeed while you use salbutamol. The amount in milk is too small to affect them. But if your baby is in the NICU or has heart or lung conditions, let your pediatrician know. They may monitor heart rate more closely, but stopping your inhaler is rarely necessary.
Is it safe to use salbutamol with other asthma medications while breastfeeding?
Yes. Inhaled steroids like budesonide, long-acting bronchodilators like formoterol, and combination inhalers are all considered safe during breastfeeding. Always tell your doctor what you’re using so they can check for interactions, but most asthma meds are compatible with nursing.





Comments
i mean like... how do we even know what's in the milk? they say it's 'tiny' but what if it's tiny and cumulative? like what if your baby gets 20 micrograms a day for a year? that's 7.3 milligrams. that's not nothing. and who funded these studies? big pharma? lol.
so let me get this straight... you're telling me it's safe to pump poison into my baby's body because some doctor with a clipboard says so? i've read about how beta-agonists mess with fetal heart development. why are we pretending this is harmless?
The data presented is methodologically sound and aligns with current clinical guidelines. The pharmacokinetic profile of inhaled salbutamol demonstrates negligible systemic absorption, and transmammary transfer is quantitatively insignificant. The American Academy of Pediatrics classification as L1 is evidence-based and should be the primary reference for clinical decision-making.
i just want to say thank you for writing this. i was terrified to use my inhaler after my daughter was born. i thought i was hurting her. reading that even preemies get higher doses in the NICU? that broke something in me. i started using it again last week. i slept for 5 hours straight for the first time in 6 months. she’s feeding better too. i didn’t know i needed to hear this.
Just a quick tip for anyone using a spacer: make sure you're using it right! I used to just puff into it and then breathe in - but my midwife showed me to exhale fully first, then seal my lips around it, then inhale slow and steady. That cut my throat residue by like 70%. Also, rinse with water AND spit it out - don't swallow it. And yes, using it after feeding? Total game changer. My baby used to gag when I kissed her after a puff. Now? No issues.
They say its safe... but what about the 2009 study that got buried? The one where infants exposed to inhaled beta-agonists had elevated cortisol levels? They deleted it. Why? Because it contradicts the narrative. I'm not saying don't use it... I'm saying be aware. The system doesn't want you to know the truth. And your baby's heart rate? Don't trust the monitor. I've seen it spike after a puff. You think that's normal?
Honestly, i read this whole thing and i'm just... underwhelmed. This is basic pharmacology. If you're a mother in the Global South, you don't even have access to spacers. And yet you're lecturing about 'minimal exposure'? The real issue is systemic neglect. Why are we optimizing for privileged mothers with inhalers and spacers while others are using expired generics from street pharmacies? This feels like virtue signaling with a stethoscope.
There’s a deeper truth here, isn’t there? We’re conditioned to fear the chemical, but not the silence. The silence of a mother gasping for air at 3 a.m. The silence of a baby crying because mom’s too tired to hold her. The silence of a milk supply vanishing because anxiety is a worse drug than any inhaler. Salbutamol isn’t the villain - the guilt is.
I used salbutamol every time I sneezed for 14 months. My son is now 3. He runs, climbs, laughs. No issues. Don't overthink it. Breathe. Feed. Repeat.