When your insurance denies your brand-name medication because a generic is available, but that generic makes you feel worse-or doesn’t work at all-you’re not alone. Thousands of people face this every year. It’s not about wanting the more expensive option. It’s about survival. For some, switching to a generic isn’t just inconvenient-it’s dangerous.
Why a Generic Might Not Work for You
Generics are required by the FDA to deliver 80% to 125% of the active ingredient found in the brand-name drug. Sounds fair, right? But that 45% window matters. For drugs with a narrow therapeutic index-like levothyroxine, warfarin, or certain seizure medications-even small differences in absorption can cause serious problems. Take thyroid medication. One patient in Brisbane reported their TSH levels jumped from 2.1 to 14.7 after switching to a generic levothyroxine. Symptoms? Fatigue, weight gain, brain fog. Their doctor confirmed: the generic wasn’t controlling their condition. The FDA doesn’t test how each person reacts to different fillers or coatings in generics. Those inactive ingredients-dyes, binders, preservatives-can trigger allergies, digestive issues, or even neurological reactions in sensitive people. Studies show 15-20% of patients on certain drug classes experience therapeutic failure with generics. That’s not rare. It’s common enough that the American Medical Association has called it a public health issue. And if you’re one of them, your insurance doesn’t always care-until you fight back.The Appeal Process: What You Need to Know
Your insurance won’t approve your brand-name drug on a hunch. They need proof. Here’s how the process works:- You get a denial letter. It’ll say something like “Generic available” or “Not on formulary.”
- You have 180 days to file an internal appeal with your insurer (60 days for Medicare Part D).
- If denied again, you can request an external review by an independent third party.
- For Medicare, there are up to five levels of appeal-including a hearing with an administrative law judge.
How to Win Your Appeal
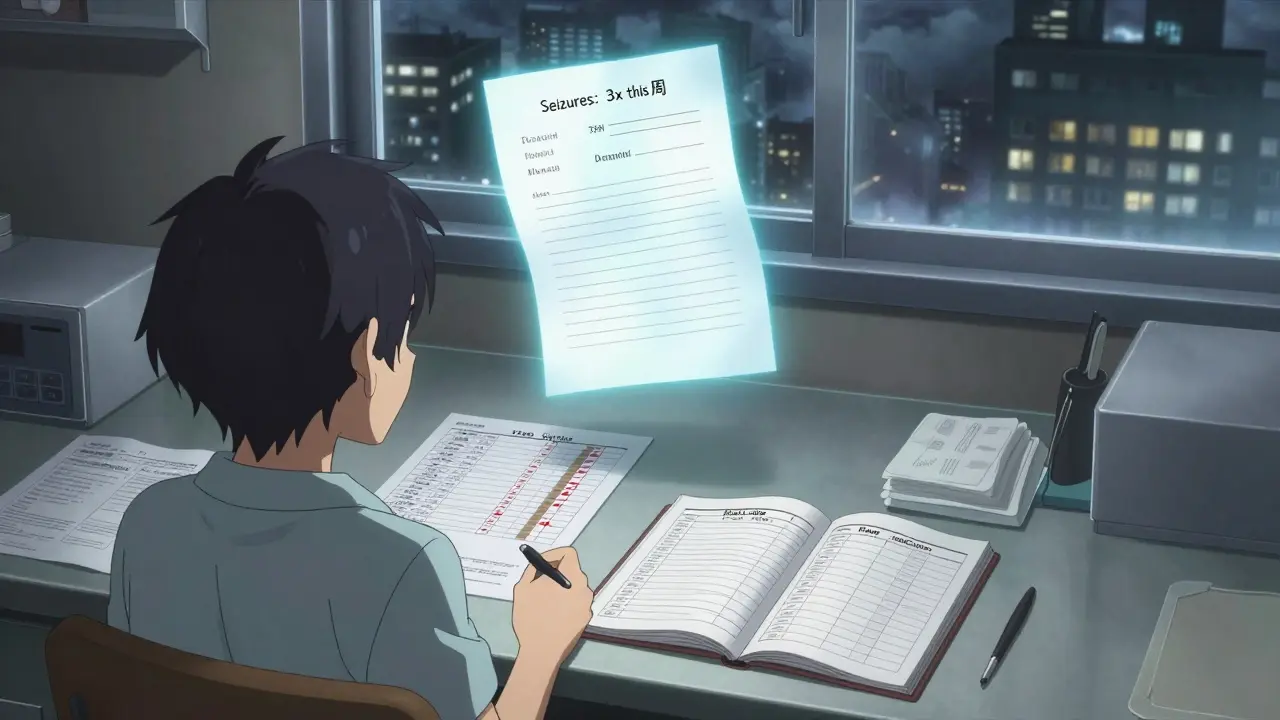
Successful appeals share three things: clear evidence, specific language, and timing. 1. Track your symptoms. Keep a daily log. Note when you switched meds, what symptoms appeared, and how bad they got. Did your seizures increase? Did your anxiety spike? Did your blood pressure become unstable? Write it down. Use a notebook, an app, or a spreadsheet. Insurers respond to patterns. 2. Get lab results. Blood tests are gold. If you’re on levothyroxine, show them your TSH, T3, T4 levels before and after the switch. If you’re on warfarin, show INR values. A TSH level of 14.7 isn’t “a little off”-it’s life-threatening. That’s not opinion. That’s science. 3. Get a detailed letter from your doctor. This isn’t a form letter. It needs to say:- Why the brand-name drug is medically necessary
- What happened when you tried the generic (symptoms, lab changes, hospital visits)
- Why other generics won’t work either
- Which guidelines support your case (like the Endocrine Society’s stance on thyroid meds)
What Works Best: Real Examples
One man in Queensland with epilepsy had breakthrough seizures every time he switched generics. His neurologist submitted a letter citing his EEG results, seizure frequency logs, and a 2023 study from Epilepsia showing different brain activation patterns with generic levetiracetam. Approval: granted. A woman with Crohn’s disease tried three biosimilars after her biologic was denied. Each one caused flare-ups. Her appeal included dates, doses, and colonoscopy reports. Approved on the third try. These aren’t outliers. They’re the rule when you document properly.Where the System Fails
Insurers often demand you try multiple generics before approving the brand. Some even require six months of failure. That’s dangerous. For someone with epilepsy or heart disease, waiting six months isn’t patience-it’s risk. Twenty-eight states now ban this “step therapy” for documented therapeutic failure. But Queensland doesn’t have that law yet. So you have to push harder. Another trick: insurers sometimes claim “no clinical evidence exists” when you’ve provided it. That’s when you escalate. External reviewers don’t work for your insurance company. They’re neutral. And they overturn denials 67% of the time when the paperwork is solid.
Tools and Support That Help
You don’t have to do this alone.- GoodRx Appeal Assistant generates a customizable appeal letter your doctor can sign in minutes. Over 147,000 appeals were processed through it in 2023-with a 68% success rate.
- Patient Advocate Foundation offers free case managers who help you gather records and write letters. Their 2023 report showed 92% satisfaction among users.
- OptumRx and Accredo (specialty pharmacies) have dedicated appeal teams. Their patients see approval rates of 73%-compared to 51% for those who go it alone.
What’s Changing in 2026
The system is slowly improving. In 2024, CMS mandated that insurers process appeals for anti-seizure drugs within 72 hours. The FDA is exploring new guidelines that recognize individual differences in how generics are absorbed. And 19 states now have “right to try brand” laws-meaning after two failed generics, insurers must approve the original. But here’s the truth: until you speak up, nothing changes. The insurance companies aren’t out to hurt you. They’re following cost-cutting rules written by bureaucrats who’ve never had a seizure from a generic pill. You’re the expert on your own body. Your doctor is the expert on your health. Together, with the right paperwork, you can win.Getting Started Today
1. Find your denial letter. Look for codes like DA2000 or DA1200. 2. Pull your lab results from the last 3 months. 3. Schedule a 30-minute appointment with your doctor. Bring your symptom log. 4. Ask them to write a letter using the exact language from the FDA and AMA guidelines. 5. Submit your appeal within 180 days. Don’t wait. This isn’t about fighting the system. It’s about making sure the system works for you.What if my doctor won’t help with the appeal?
Many doctors are overwhelmed-but most will help if you make it easy. Bring them your symptom log, lab results, and a template letter from GoodRx or the Patient Advocate Foundation. Most will sign it with minimal changes. If they refuse, ask for a referral to a specialist or contact your state’s medical board for guidance.
How long does the appeal process take?
Internal appeals take 14-30 days. External reviews take 30-45 days. For urgent cases-like seizure risk or heart instability-you can request an expedited review. Medicare must respond within 72 hours. Don’t assume it’ll be fast; plan for delays and keep your current meds stocked if possible.
Can I get my brand-name drug while waiting for approval?
Sometimes. Ask your pharmacy if they offer a short-term bridge supply through a manufacturer’s patient assistance program. Companies like AbbVie, Pfizer, and Teva often have free or low-cost programs for patients in transition. You can also ask your doctor for a 30-day emergency prescription while your appeal is pending.
Why do some people get approved and others don’t?
It’s not luck. It’s documentation. Appeals with lab data, symptom logs, and physician letters citing clinical guidelines have an 82% approval rate. Appeals with vague statements like “I feel better on the brand” get denied 90% of the time. Insurers respond to evidence, not emotion.
Is this only for expensive drugs?
No. This applies to any medication where therapeutic failure is documented-whether it’s a $10 generic or a $10,000 biologic. The issue isn’t cost. It’s safety. Even low-cost drugs like gabapentin or levothyroxine can cause serious harm if the generic formulation doesn’t work for you.
What if my appeal is denied again?
Keep going. Most approvals happen at the external review stage. If you’re on Medicare, you can appeal to the Office of Medicare Hearings and Appeals. If you’re on private insurance, you can request a state-level external review. Each level gives you another chance. Don’t give up after the first denial.





Comments
It’s fascinating how the FDA’s 80%-125% bioequivalence window is treated as a universal constant, when human physiology varies so wildly. I’ve seen patients on levothyroxine whose TSH levels swing like a pendulum just because the generic manufacturer switched from lactose to cornstarch as a binder. The system assumes uniform absorption, but absorption isn’t just about the active ingredient-it’s about mucosal pH, gut flora, even bile salt concentration. No one’s testing that. And yet, we’re expected to treat generics as interchangeable widgets. It’s not negligence-it’s systemic reductionism.
Let’s be real: this isn’t about medicine. It’s about capital’s triumph over corporeality. The pharmaceutical-industrial complex has commodified biological variance into a cost-center optimization problem. Generics? They’re the neoliberal answer to suffering-cheap, standardized, and emotionally inert. The patient’s lived experience is reduced to a line item in an actuarial spreadsheet. We’ve turned healing into a spreadsheet function. And the worst part? We’ve all internalized this. We don’t even scream anymore-we just file appeals.
This is very important. I come from India, where many people rely on generics because they can’t afford brand names. But I’ve seen friends suffer when generics didn’t work-same medicine, different result. It’s not about money. It’s about trust. If your body reacts badly, you deserve to be heard. Doctors should listen, and insurance should care. Not because it’s expensive, but because it’s human.
Bro… I switched generics for my anxiety med and felt like my brain was full of static 😵💫. Took me 3 months to get my doc to write the letter. Insurance said ‘nope’ twice. Then I sent them my sleep tracker data + my therapist’s note + a screenshot of my panic attack log. They approved it on the third try. Don’t give up. You’re not crazy. The system is.
Thank you for writing this. I’ve been through this with my daughter’s seizure meds. The first time she got switched to generic levetiracetam, she had three seizures in 48 hours. We had to rush to the ER. The nurse said, ‘It’s just a generic, it’s supposed to be the same.’ I cried in the parking lot. This post? It’s the kind of thing that makes people feel less alone. Please keep sharing these stories. And if you’re reading this and you’re fighting this battle-you’re doing amazing work.
Documentation is the only language insurers understand. Clinical evidence, not anecdotes. Precision, not passion. The system is flawed, but it is navigable. Follow the protocol. Submit the data. Escalate. There is no emotional shortcut.
I’ve spent years watching people get crushed by this. Not because they’re weak, but because the system is designed to exhaust them. The appeal process isn’t a right-it’s a marathon with no finish line marked. You have to be part patient, part paralegal, part data analyst. And even then, you’re at the mercy of a bureaucrat who’s never held a pill in their hand. The real tragedy isn’t the denial. It’s that we’ve normalized this as just part of being sick.
Y’all need to know: GoodRx’s appeal tool is a GAME CHANGER. I used it for my dad’s warfarin. He was bleeding internally because his INR kept spiking after the switch. Doc was overwhelmed, so I used the template, filled in his labs, printed it, and handed it to him. He signed it in 5 minutes. Approved on the first try. No drama. No stress. Just science + a good template. Do it. Save yourself the headache.
My sister had a severe allergic reaction to the dye in a generic version of gabapentin. Swelling, hives, near-anaphylaxis. Turns out, the dye wasn’t listed on the label because it’s an ‘inactive ingredient.’ No one tells you that. No one warns you. I spent weeks digging through FDA MedWatch reports. Found 12 other cases just in our state. We filed a complaint. They changed the labeling. Small win. But it matters.
Let’s cut the sentimentality. This isn’t a moral crisis. It’s a market failure. Patients who can’t afford brand-name drugs should pay less. But if you’re claiming a generic doesn’t work, you’re not a victim-you’re a statistical outlier. The data is clear: 80% of patients do fine. The rest? They’re either misdiagnosed, non-compliant, or seeking a premium experience under the guise of medical necessity. Stop gaslighting the system. Fix your diagnosis first.
THIS IS WHY WE CAN’T HAVE NICE THINGS. Big Pharma and the FDA are in bed with insurers. They don’t care if you have seizures. They care if your insurance premium goes up. They’re letting people die so they can save $2.37 per pill. And you think your appeal matters? It doesn’t. They’ll just deny it again and again until you give up. This isn’t broken-it’s BY DESIGN. Wake up.
Documentation wins. Always.
They’re replacing our meds with Chinese generics because the government wants to weaken American health sovereignty. You think this is about cost? It’s about control. The FDA doesn’t test these pills properly. They’re getting shipped through ports that don’t even check for contaminants. This isn’t medicine-it’s a bio-weapon disguised as savings. You think your TSH is the only thing changing? Wait until your liver starts failing.
They’re putting fluoride in the generics to make us docile. I read it on a blog. My cousin’s cat got sick after eating a crushed pill. Coincidence? I think not. Also, the FDA is owned by Pfizer. Don’t believe the hype. Fight back. Don’t take the pill. Go raw. Or better yet-move to Canada.