Antiparasitic Drug Selector
Recommended Treatment Option
Drug 1
Drug 2
When you hear the name Ivermectin comparison, you probably picture a single pill that clears everything from head lice to river blindness. The reality is messier: Ivermectol (Ivermectin) is one of many antiparasitic agents, each with its own strengths, weaknesses, and approved uses. This guide breaks down the most common alternatives-Moxidectin, Albendazole, Milbemycin oxime, and Nitazoxanide-so you can see where Ivermectol shines and where another drug might be the better choice.
What Is Ivermectol?
Ivermectol is a broad‑spectrum antiparasitic medication that belongs to the macrocyclic lactone class. It works by binding to glutamate‑gated chloride channels in the nerve and muscle cells of invertebrates, causing paralysis and death of the parasite. First approved for veterinary use in the early 1980s, it gained human approval in 1987 for onchocerciasis (river blindness) and later expanded to treat strongyloidiasis, scabies, and certain lice infestations.
Key Criteria for Comparing Antiparasitic Drugs
- Efficacy: How well the drug clears the targeted parasite.
- Safety profile: Frequency and severity of adverse events.
- Approved indications: What diseases regulators allow the drug for.
- Dosing convenience: Number of doses and need for weight‑based calculations.
- Cost and accessibility: Price per treatment course and availability in low‑resource settings.
Alternative #1: Moxidectin
Moxidectin is another macrocyclic lactone, chemically similar to Ivermectol but with a longer half‑life (up to 30 days). It was initially a veterinary drug before receiving FDA approval in 2018 for onchocerciasis in adults, offering a single‑dose regimen.
When it’s better: The prolonged half‑life means fewer repeat doses for diseases that require multiple rounds, such as onchocerciasis in endemic regions. Its efficacy against Onchocerca volvulus is comparable to Ivermectol, but with higher cure rates after one dose.
Drawbacks: Limited approval outside of onchocerciasis; less data on safety in pregnant women and children under 12. Cost per tablet is higher in most markets.
Alternative #2: Albendazole
Albendazole belongs to the benzimidazole class and works by inhibiting microtubule formation in parasites. It is orally active and is the drug of choice for soil‑transmitted helminths such as Ascaris, hookworm, and Trichuris.
When it’s better: For broad‑spectrum deworming campaigns targeting multiple helminths, Albendazole’s coverage is wider than Ivermectol’s. It also penetrates tissues well, making it effective against neurocysticercosis.
Drawbacks: Less potent against ectoparasites like scabies or lice. Rare but serious liver toxicity can occur with prolonged use.
Alternative #3: Milbemycin Oxime
Milbemycin oxime is a macrocyclic lactone related to Ivermectol, commonly used in veterinary medicine for heartworm and intestinal parasites. Human formulations are not widely available, but research is ongoing for its use in strongyloidiasis.
When it’s better: In regions where Ivermectol resistance has emerged in animal parasites, Milbemycin may retain activity. Its safety margin is slightly higher in dogs, suggesting a potential for lower neurotoxicity.
Drawbacks: Lack of regulatory approval for human use limits clinical application. Data on pharmacokinetics in humans are sparse.
Alternative #4: Nitazoxanide
Nitazoxanide is a thiazolide that interferes with the pyruvate:ferredoxin oxidoreductase enzyme pathway of parasites and some anaerobic bacteria. It is approved for cryptosporidiosis and has off‑label use for Giardia.
When it’s better: For diarrheal diseases caused by protozoa, Nitazoxanide outperforms Ivermectol, which has limited activity against Giardia and no effect on Cryptosporidium.
Drawbacks: Less effective against helminths; side effects include mild gastrointestinal upset and a metallic taste.
Side‑by‑Side Comparison Table
| Attribute | Ivermectol (Ivermectin) | Moxidectin | Albendazole | Milbemycin oxime | Nitazoxanide |
|---|---|---|---|---|---|
| Drug class | Macrocyclic lactone | Macrocyclic lactone | Benzimidazole | Macrocyclic lactone | Thiazolide |
| Half‑life | 12-36 hrs | ~30 days | 3-5 hrs | ~24 hrs (animal data) | 1-4 hrs |
| Primary approved uses (human) | Onchocerciasis, strongyloidiasis, scabies, lice | Onchocerciasis (single dose) | Soil‑transmitted helminths, neurocysticercosis | Investigational (strongyloidiasis) | Cryptosporidiosis, Giardia (off‑label) |
| Typical dose | 200µg/kg, single or repeat | 8mg/kg, single | 400mg single | Not established | 500mg twice daily × 3 days |
| Common side effects | Mild fever, itching, headache | Rare neuro‑toxicity, nausea | Liver enzyme rise, abdominal pain | Generally well tolerated in animals | GI upset, metallic taste |
| Cost (U.S. retail, 2025) | $0.10‑$0.20 per 3mg tablet | $0.30‑$0.45 per 3mg tablet | $0.05‑$0.07 per 400mg tablet | Not commercially available | $1.00‑$1.50 per 500mg tablet |
Safety Considerations Across the Board
All five drugs have a good safety record when used as directed, but the risk profile shifts with age, pregnancy, and co‑administered medicines.
- Ivermectol: Contraindicated in patients with known hypersensitivity. Neurological adverse events are rare but have been reported at high doses or in patients with Loa loa infection.
- Moxidectin: Limited data in pregnancy; animal studies suggest caution.
- Albendazole: Teratogenic risk in the first trimester; liver function monitoring advised for prolonged therapy.
- Milbemycin oxime: No human safety data; theoretical neurotoxicity similar to other macrocyclic lactones.
- Nitazoxanide: Generally safe; avoid in severe hepatic impairment.

How to Choose the Right Drug for Your Situation
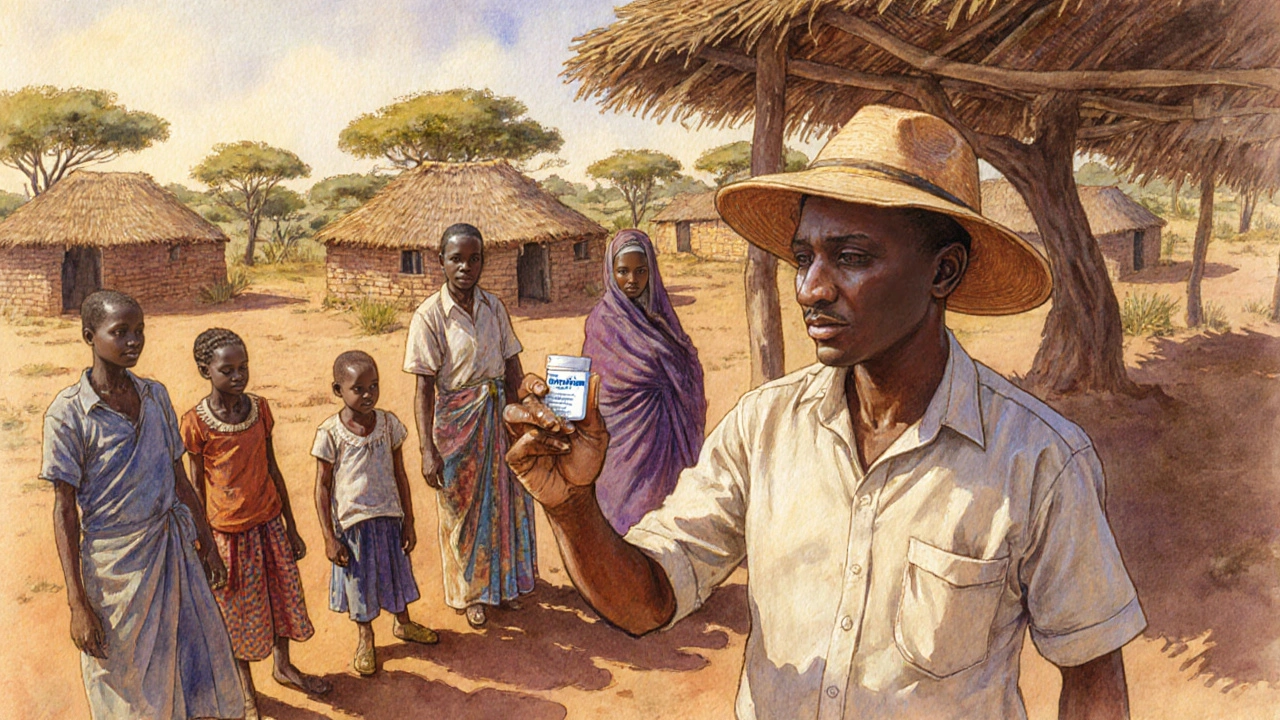
Imagine you’re a field health worker in a remote African village. You have a limited stock of medicines, must treat onchocerciasis, and need a regimen that requires just one visit. In that scenario, Moxidectin often wins because a single dose can clear the infection and you avoid the logistical nightmare of a second visit for Ivermectol.
Now picture a community health center in Southeast Asia facing a wave of soil‑transmitted helminths among schoolchildren. Albendazole becomes the go‑to drug because it hits multiple worm species with a single dose, keeping the program simple and cheap.
For an urban clinic dealing with stubborn scabies outbreaks, Ivermectol’s proven efficacy and easy topical formulation make it the first choice, while Nitazoxanide would be irrelevant.
So the decision tree looks like this:
- Identify the parasite (or group of parasites) you need to target.
- Check regulatory approval for the indication in your country.
- Consider dosing convenience (single vs. multiple doses).
- Weigh safety in the specific patient population (children, pregnant women, liver disease).
- Factor in cost and supply chain reliability.
Emerging Research and Future Directions
In 2024, a large multicenter trial compared a single 12mg dose of Ivermectol to a 8mg/kg dose of Moxidectin for onchocerciasis. The study showed non‑inferior efficacy for Moxidectin but highlighted a slightly higher rate of mild dizziness. Researchers are also exploring combination therapies-pairing Ivermectol with doxycycline to target Wolbachia bacteria in filarial infections, which could improve cure rates.
Albendazole is being reformulated into chewable tablets for preschool children, aiming to increase compliance. Meanwhile, Nitazoxanide is under investigation for its antiviral properties, though results are still early and not ready for clinical use.
Practical Tips for Prescribers and Patients
- Always verify the weight‑based dose for Ivermectol; an overdose can increase neuro‑toxicity risk.
- If the patient has a high Loa loa microfilarial load, avoid Ivermectol and consider albendazole with steroids.
- Store tablets away from moisture and heat; most macrocyclic lactones degrade quickly in humid climates.
- For pediatric dosing, split tablets only if a scored tablet is available; otherwise use a liquid formulation to ensure accuracy.
- Educate patients that side effects like mild itching often mean the drug is working-parasites are dying and releasing antigens.
Bottom Line
Ivermectol remains a versatile, low‑cost workhorse for many parasitic diseases, but it isn’t the universal answer. Moxidectin offers a single‑dose edge for onchocerciasis, Albendazole covers a broader worm spectrum, Milbemycin stays in the research lane, and Nitazoxanide fills the gap for protozoal diarrheal illnesses. By matching the drug’s strengths to the patient’s needs, you’ll get the best cure rates while minimizing side effects and costs.
Frequently Asked Questions
Can I use Ivermectol for COVID‑19?
Current high‑quality trials have not demonstrated a consistent benefit of Ivermectol for COVID‑19. Major health agencies, including the WHO and FDA, advise against its use outside of approved clinical trials.
Is Moxidectin safe for children under 12?
Moxidectin is approved for adults and adolescents 12years or older. Data in younger children are limited, so clinicians usually prefer Ivermectol or Albendazole for that age group.
What is the main advantage of Albendazole over Ivermectol?
Albendazole’s broader spectrum covers multiple soil‑transmitted helminths in a single dose, making it ideal for mass deworming programs that target Ascaris, hookworm, and Trichuris simultaneously.
Are there any drug interactions with Ivermectol?
Ivermectol is metabolized by CYP3A4. Strong inducers (e.g., rifampicin) can lower its levels, while inhibitors (e.g., ketoconazole) may raise concentrations, potentially increasing side‑effect risk.
Which drug is cheapest for treating scabies?
Ivermectol, either as a single oral dose or as a topical cream, is generally the most affordable option worldwide, often priced under $0.20 per tablet in generic form.







Comments
Ivermectin is cheap but not a magic bullet.
The table shows cost, half‑life, and dosing; the differences matter, especially in low‑resource settings; still, clinicians need to weigh safety, efficacy, and logistics.
Pharmacokinetic parameters such as Cmax and AUC for ivermectin demonstrate a dose‑dependent exposure profile, whereas moxidectin exhibits a markedly prolonged terminal half‑life, thereby reducing the frequency of administration required for sustained parasitic clearance.
Remember, matching the drug to the patient’s situation can really make a difference.
Oh yeah, because we all love paying extra for a drug that does the same thing.
Esteemed colleagues, it is incumbent upon us to scrutinise the pharmacodynamic profile of moxidectin-its prolonged half‑life confers dosing convenience, yet its limited indication restricts utility.
One must not overlook the subtle interplay of CYP‑mediated metabolism; overlooking such nuance would be an egregious oversight.
We shouldnt just take the cheap pills without thinkin about the long term effects.
Great rundown! For anyone treating scabies, ivermectin remains the go‑to because it's affordable and effective.
Seriously, if you think a single table can replace years of clinical experience, you’re living in a fantasy world.
The epistemic value of such comparative analyses is, undeniably, profound-though oft en the layman’s eye remains blind.
When selecting an antiparasitic, the clinician must first delineate the specific parasite involved.
This determination drives the choice of drug more than any other factor.
Efficacy data, such as cure rates reported in randomized trials, should be examined critically.
Safety considerations, including known neurotoxic risks, are paramount for vulnerable populations.
Cost analysis cannot be ignored in low‑resource settings where budget constraints dictate formularies.
For onchocerciasis, the single‑dose regimen of moxidectin offers logistical advantages over multi‑dose ivermectin.
However, moxidectin’s regulatory approval is limited to adults, making ivermectin the fallback for children.
In cases of soil‑transmitted helminths, albendazole’s broad spectrum surpasses ivermectin’s more narrow activity.
When treating scabies, ivermectin’s oral formulation complements topical therapy and accelerates resolution.
Nitroazoxanide should be reserved for protozoal diarrheas, as its effect on helminths is negligible.
The physician must also assess comorbidities such as liver disease that may alter drug metabolism.
Drug interactions, especially with CYP3A4 inducers or inhibitors, can modify plasma concentrations.
Patient adherence improves when dosing schedules are simple, reinforcing the appeal of single‑dose options.
Ultimately, a balanced decision integrates clinical evidence, patient characteristics, and supply chain realities.
By applying this multifaceted framework, health workers can maximize therapeutic success while minimizing adverse outcomes.
Keep it simple, choose the drug that fits your patient’s needs and budget.
I wonder how the new chewable albendazole will impact child compliance-maybe a game changer?
Dear readers!!! The battle between macrocyclic lactones is nothing short of an epic saga!!!
In conclusion, the selection of an antiparasitic agent should be guided by evidence‑based criteria, including efficacy, safety, and accessibility.
Wow-what a vivid tapestry of drug profiles! Each option shines like a different hue on the palette of parasitic therapy!