Most people assume that if a pill is past its expiration date, it’s just useless-like old milk or stale bread. But with antibiotics, the stakes are higher. Taking an expired antibiotic might not just mean your infection doesn’t go away. It could make things worse-by fueling superbugs that no drug can touch.
What Does an Expiration Date Actually Mean?
Expiration dates aren’t random. They’re the last day the manufacturer guarantees the drug will work exactly as labeled-100% potency, zero risk of harmful breakdown products. This isn’t a guess. It’s based on strict stability testing required by the FDA since 1979. But here’s the twist: that date doesn’t mean the medicine suddenly turns toxic or useless the next day.
A massive U.S. government study called the Shelf Life Extension Program tested over 3,000 lots of drugs, including antibiotics, stored under ideal conditions. The results? About 90% of them still had at least 90% of their original strength-even 15 years after expiration. That’s not a fluke. It’s science.
But here’s the catch: those were controlled, lab-perfect conditions. Your bathroom cabinet? Not even close.
Not All Antibiotics Are Created Equal
Some antibiotics hold up way better than others. Solid forms-tablets and capsules-like amoxicillin, cephalexin, or doxycycline, are generally stable. HPLC testing shows they often retain 85-92% potency even a year past their date, as long as they’re kept dry and cool.
Liquid antibiotics? Big problem.
Amoxicillin suspension, the kind given to kids, starts falling apart fast. At room temperature, it can lose nearly half its strength within a week after expiration. Ceftriaxone, used in hospitals, degrades even under refrigeration. Beta-lactam antibiotics like penicillin and amoxicillin are especially sensitive to moisture and heat. Once they break down, they don’t just get weaker-they can turn into compounds that trigger allergies or promote resistant bacteria.
And here’s the scary part: you won’t always know. A 2021 study found that 89% of degraded antibiotics showed no visible changes-no cloudiness, no smell, no color shift. That’s why tasting a pill or checking its appearance won’t save you.
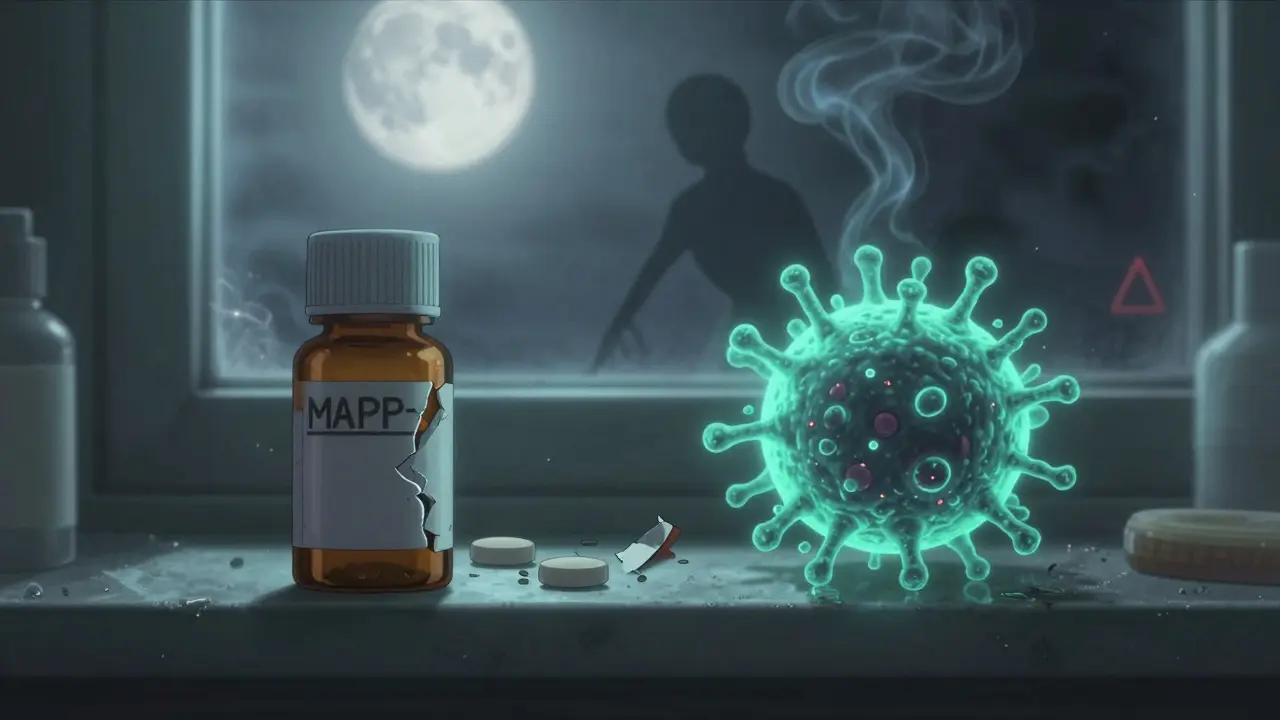
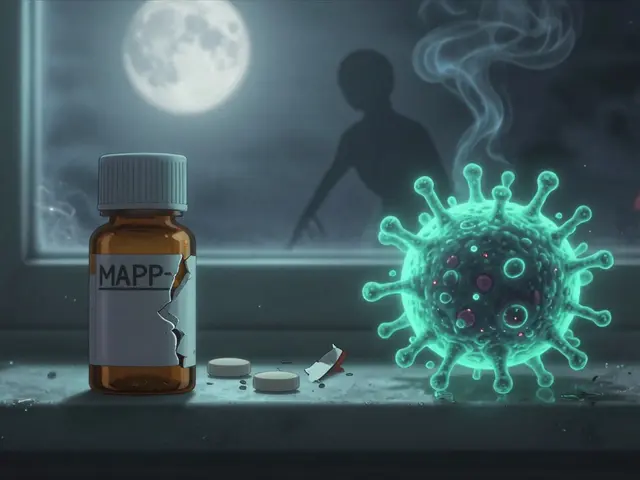
Why Taking Expired Antibiotics Can Make Resistance Worse
Antibiotics aren’t like painkillers. If you take too little, you don’t just feel worse-you train bacteria to survive.
When an expired antibiotic loses potency, it doesn’t kill all the bacteria. It knocks them down, weakens them, but leaves the toughest ones alive. Those survivors multiply. And now you’ve got a strain that’s harder to treat-not just for you, but for everyone.
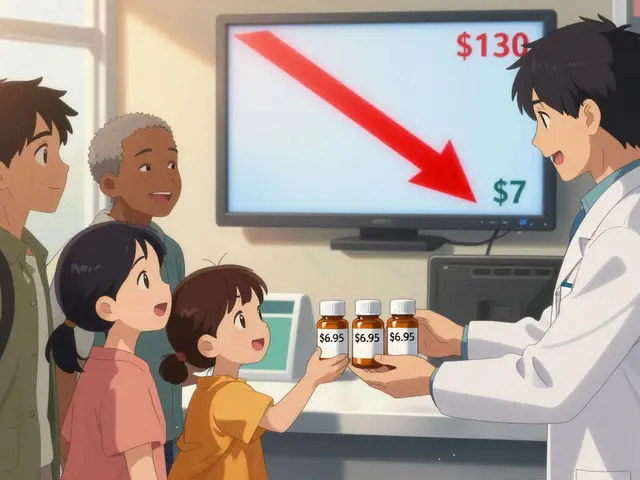
Research from 2023 analyzed over 12,850 patient cases. It found that expired pediatric antibiotics led to resistance rates of 98.7% against common infections like E. coli. Compare that to 14.3% with fresh meds. The minimum dose needed to kill those bugs jumped from 0.5 μg/mL to a whopping 256 μg/mL. That’s not a small change. That’s a public health emergency.
The Infectious Diseases Society of America warns this isn’t just about one person’s failed treatment. It’s about creating superbugs that spread through communities. And it’s happening right now.

What Experts Actually Say
The FDA says: don’t use expired drugs. Full stop. Their official stance is clear: potency and safety can’t be guaranteed.
But some doctors and pharmacists see it differently-especially when there’s a shortage.
Dr. Lee Cantrell from UC San Diego says, in a crisis, properly stored solid antibiotics might still work 12-24 months past expiration. Johns Hopkins Hospital has a protocol that extends expiration dates for 14 critical antibiotics during shortages. They’ve treated over 2,300 patients this way-with zero failures linked to potency.
The European Medicines Agency takes a middle ground: solid antibiotics might be okay for 6-12 months past expiration if stored right. But they draw a hard line: never use expired liquids, especially for serious infections like pneumonia or sepsis.
So who’s right? It’s not black and white. But here’s the bottom line: if you’re sick enough to need an antibiotic, you shouldn’t gamble with an expired one.
Real People Are Taking Expired Antibiotics-And It’s Backfiring
On Reddit, 63% of users admitted to taking expired antibiotics. Most did it for colds, sinus infections, or UTIs. Nearly 70% said their symptoms didn’t fully go away. Over 20% ended up in the ER.
A 2022 survey of over 2,000 people found that 78% couldn’t tell if an antibiotic had gone bad just by looking at it. And 63% thought cloudiness meant it was useless-when in reality, many degraded pills look perfectly fine.
In low-income countries, it’s even worse. Nearly 90% of pharmacies still sell antibiotics within 3 months of expiration. Some knowingly give out expired ones during shortages. The result? Treatment failure rates are 18% higher than in places with reliable stock.
This isn’t resourcefulness. It’s a slow-motion crisis.
How to Store Antibiotics to Maximize Their Life
If you’re keeping antibiotics around-whether you plan to use them or not-storage matters more than you think.
Keep them in their original bottle, with the desiccant packet still inside. Store them in a cool, dry place-like a bedroom drawer, not the bathroom. Humidity and heat are their worst enemies.
Studies show antibiotics stored at 15-25°C with 35-45% humidity last 37% longer than those in a steamy bathroom (where average temp hits 28.7°C and humidity is 72%). That’s months of extra potency.
And never transfer pills to pill organizers unless you’re using them right away. Those containers expose meds to air and moisture, speeding up degradation.
When Might It Be Okay to Use an Expired Antibiotic?
Let’s be real: sometimes, you’re stuck. No pharmacy open. No money for a new prescription. You’ve got a mild sinus infection and an old amoxicillin bottle from last year.
The CDC and the Antibiotic Resistance Leadership Group say: for non-life-threatening conditions, you *might* consider it-if three things are true:
- The antibiotic is a solid tablet or capsule (not liquid).
- It’s been stored properly-cool, dry, sealed.
- It’s no more than 12 months past expiration.
And even then: check for damage. Crumbling? Discolored? Smells weird? Toss it. Don’t risk it.
But if you’re dealing with a fever, chest pain, ear infection in a child, or any sign of something serious-go to a doctor. Don’t gamble with expired meds. The risk of resistance isn’t worth it.
What’s Changing? The Future of Expiration Dates
The system is outdated. We’re stuck with fixed dates, but drugs don’t expire like milk. Their stability depends on how they’re stored, their formulation, and even the humidity in your house.
That’s why the FDA is testing a new pilot program: using rapid tests to extend expiration dates during shortages. IBM and the FDA are working on AI tools that predict how long a specific pill will last based on its storage history. Imagine scanning a bottle and getting a real-time potency estimate.
Researchers at the University of Illinois have already created paper test strips that detect if amoxicillin has lost potency-with 94.7% accuracy. They’re not on shelves yet, but they’re coming.
For now, though, the safest rule is simple: if you’re unsure, don’t take it.
What Should You Do With Expired Antibiotics?
Don’t flush them. Don’t throw them in the trash where kids or pets might get them. Don’t give them to a friend.
Find a drug take-back program. Many pharmacies, hospitals, and police stations have drop boxes. If that’s not available, mix pills with coffee grounds or cat litter, seal them in a bag, and throw them in the trash. It’s not perfect-but it’s safer than leaving them lying around.
And next time you fill a prescription, ask your pharmacist: "How long will this last if I store it right?" Most don’t know-but they should. And you deserve to know too.




Comments
So like, i read this and i’m just sitting here wondering how many people are taking their kid’s leftover amoxicillin for a sinus thing and then blaming the doctor when it doesn’t work. i mean, we all do it. but damn. the resistance stats are wild.
Let’s be clear: the Shelf Life Extension Program data is irrelevant to real-world storage. HPLC stability under controlled conditions ≠ your bathroom drawer at 80% humidity. The FDA’s warning exists for a reason. Degradation kinetics aren’t linear, and beta-lactam hydrolysis products are immunogenic. You don’t get to cherry-pick science when your life’s on the line.
wait so if its in a dry drawer and its just 6 months past exp, its kinda okay? i thought it was a hard no. also i always forget to keep the desiccant packet. oops.
In India, we have no choice. Pharmacies sell expired antibiotics because they have no stock. People die because they can’t afford new prescriptions. This is not negligence. This is systemic failure. The West talks about superbugs while ignoring the global reality of access.
Wow. So the FDA is just being overly cautious? And some random doctors are playing hero by extending expiration dates? This is like saying "my cousin’s garage mechanic fixed my transmission, so why do I need a dealership?"
Expired antibiotics don’t kill bacteria. They just make them mad.
Okay but what if you’re in a cabin in the woods with a UTI and your last dose is 14 months past expiry and it’s been stored in a sealed tin in a cool cave? Are you just supposed to wait for sepsis? The real villain here is the pharmaceutical industry’s profit-driven expiration dates, not people trying to survive.
Amoxicillin isn’t magic. It’s a molecule. Molecules degrade. Stop romanticizing it.
We are all just temporary vessels for bacterial evolution. The antibiotics we take today are the seeds of tomorrow’s unstoppable plagues. We think we’re saving ourselves-but we’re just feeding the machine.
Always talk to your pharmacist. They want to help. And if you’re unsure, just wait a day and see a doctor. You’re worth it. 💪
so like i had some doxycycline from 2022 in my nightstand and used it for a sore throat last winter and it worked fine. i dont think science should dictate how we live. also i hate when people say "dont take expired meds" like its a moral crime. chill.
Anyone who takes expired antibiotics without understanding pharmacokinetics is a liability to public health. You’re not being resourceful-you’re contributing to the collapse of modern medicine. Your ignorance is not a virtue.
So the government is lying to us again. Of course they say don’t use expired drugs-they want you to keep buying them. This is just Big Pharma gaslighting. I’m not taking their pills anymore.
i read this and i just felt really sad. like, people are trying to survive and the system is broken. and now we’re all just blaming each other instead of fixing it. i dont know what to do anymore.
Okay, but have you considered that the FDA’s expiration dates are based on worst-case storage, not optimal? And that the 90% potency metric is arbitrary? And that the Shelf Life Extension Program was funded by the DoD, which has a vested interest in stockpiling drugs? And that the entire pharmaceutical industry profits from planned obsolescence? And that no one ever tests the actual degradation products in real human bodies? And that we’ve been conditioned to fear expiration dates like they’re radioactive? And that the real problem is the lack of access to affordable healthcare, not the pills themselves? And that if we had universal healthcare, no one would be taking expired meds out of desperation? And that this whole conversation is just a distraction from the fact that medicine is a commodity, not a right? And that until we fix that, we’re just rearranging deck chairs on the Titanic?