Calcium: what it does, where to get it, and how to use supplements safely
Want stronger bones, fewer cramps, and better long-term health? Calcium is one of those nutrients you can't ignore. It builds and maintains bones and teeth, helps muscles contract, and plays a role in nerve signals and blood clotting. But too little or too much calcium causes real problems — and many people get the balance wrong.
Easy food sources and how much you need
Start with food. Dairy like milk, yogurt, and cheese are top picks. Fortified plant milks, canned salmon or sardines (with bones), tofu set with calcium, leafy greens (kale, bok choy), almonds, and fortified cereals also add up. Aim for these daily targets as a baseline: adults 19–50 — 1,000 mg; women 51+ and everyone 71+ — 1,200 mg; teens need more (about 1,300 mg). Kids and pregnant people have different needs, so check with your provider.
Note: food calcium absorbs better with a varied diet and normal vitamin D. If you’re low on dairy, combine several calcium-rich foods through the day rather than one large portion.
Smart supplement rules
If food won't cut it, use supplements—but follow a few clear rules. Pick a form that fits your stomach: calcium carbonate is cheap and works best with food; calcium citrate is gentler and OK on an empty stomach or if you take acid-reducing meds. Don’t take more than 500–600 mg of elemental calcium at one time — the gut absorbs smaller doses better. For example, split a 1,000 mg supplement into two doses.
Always check the label for "elemental calcium" — that tells you the actual amount your body gets. Also consider a product tested by a third party (USP, NSF) so you’re not getting junk fillers or heavy metals.
Vitamin D matters. Without enough D, supplemental calcium won’t absorb well. Many doctors recommend a combined approach: fix low vitamin D, then adjust calcium if needed.
Watch for drug interactions and medical warnings. Calcium can cut absorption of certain antibiotics (tetracyclines, fluoroquinolones) and thyroid meds — leave a 2–4 hour gap. People on thiazide diuretics, with kidney disease, or a history of kidney stones should check with a clinician before taking supplements. Signs of too much calcium include constipation, nausea, and in severe cases confusion or kidney issues.
Want to know if you need supplements? Ask for a blood calcium and vitamin D test. If you’re worried about bone loss, a DEXA scan tells you more than guessing. Finally, lifestyle counts: regular weight-bearing exercise, not smoking, and limiting excessive sodium and caffeine help your bones use calcium better.
Short, practical takeaway: eat calcium-rich foods first, use supplements only when needed, split doses, mind vitamin D, and space calcium from meds. When in doubt, check with your healthcare provider — small changes now pay off later.
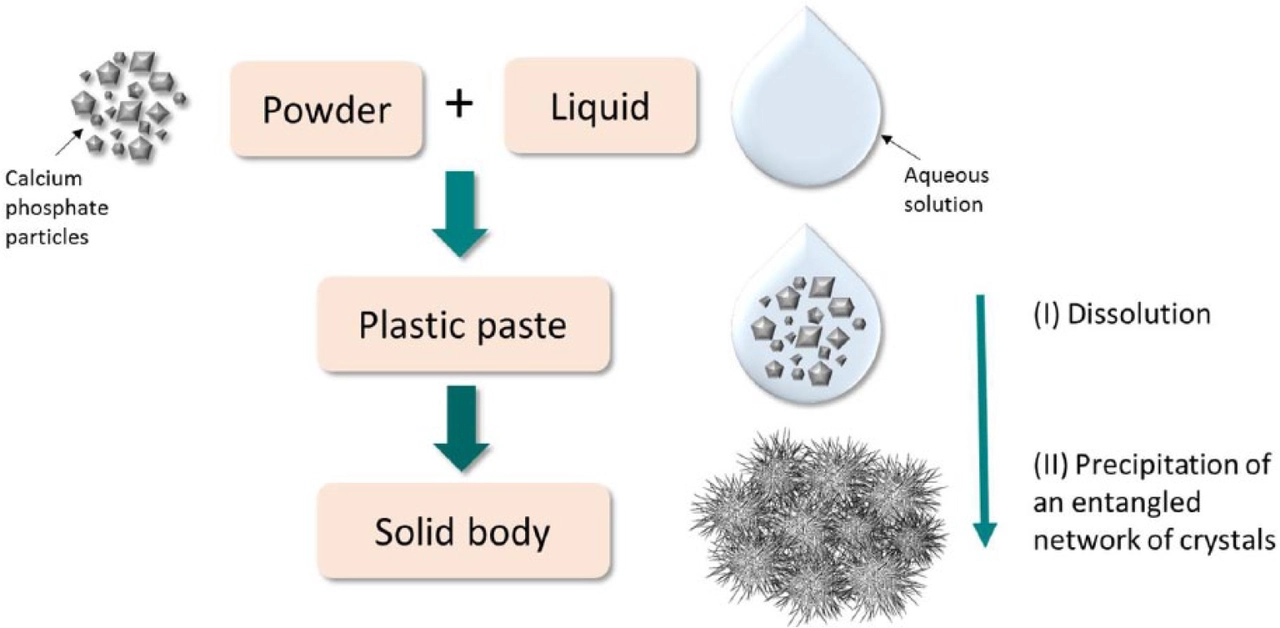
As a blogger, I've recently come across the importance of calcium and phosphorus in the development of osteodystrophy. These two minerals play a vital role in maintaining healthy bones and teeth. However, an imbalance in their levels can lead to osteodystrophy, a condition characterized by weak and deformed bones. To prevent this, it's essential to consume a balanced diet rich in calcium and phosphorus, and monitor their levels in the body. Additionally, it's crucial to consult a healthcare professional for guidance in managing these levels and maintaining overall bone health.
Read more