Infliximab Switch: What You Need to Know About Switching Biologic Drugs
When you’re on infliximab, a TNF inhibitor used to treat autoimmune conditions like Crohn’s disease, rheumatoid arthritis, and plaque psoriasis. Also known as Remicade, it works by blocking a key protein that drives inflammation. But many people eventually need to switch—whether because the drug stops working, side effects appear, or a cheaper biosimilar, a highly similar version of the original biologic drug, approved after the patent expires becomes available. An infliximab switch isn’t just changing pills; it’s a medical decision that affects your daily life, immune response, and long-term health.
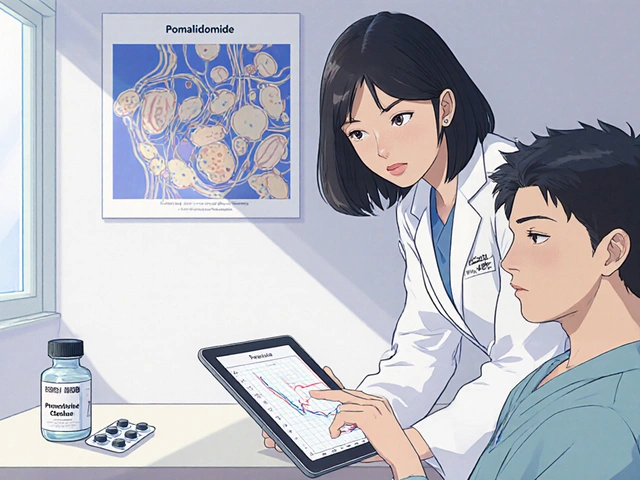
Switching from infliximab to another TNF inhibitor, a class of drugs that target tumor necrosis factor to reduce inflammation like adalimumab or etanercept is common. But it’s not always smooth. Some patients see their symptoms return quickly; others do just fine. Why? It depends on your body’s immune reaction, how long you’ve been on the drug, and whether you’re switching to a biosimilar or a different brand. Studies show that switching to a biosimilar like infliximab-dyyb or infliximab-abda often works well—up to 80% of people stay in remission. But if you’re switching to a drug from a different class, like an IL-17 or JAK inhibitor, the risks and benefits change entirely. Your doctor will look at your disease activity, past side effects, and even your insurance coverage before making a move.
Many people worry about losing control of their condition after a switch. That’s valid. But the key is planning. Don’t stop your current drug cold turkey unless your doctor says so. Most transitions involve overlapping doses or careful timing to avoid flare-ups. You’ll likely need blood tests before, during, and after the switch to check for antibodies or signs of infection. And yes, some people develop new side effects—headaches, rashes, or even rare immune reactions. That’s why tracking your symptoms in a journal helps. If your joint pain flares up two weeks after switching, or your diarrhea returns, write it down. That detail matters more than you think.
What you’ll find below are real, practical guides from people who’ve been through this. You’ll read about how one patient switched from Remicade to a biosimilar and saved $1,200 a month without losing control of their Crohn’s. Another learned the hard way why skipping lab tests after a switch was risky. There’s advice on talking to your pharmacist about drug substitutions, how to spot a fake biosimilar, and what to do if your insurance denies coverage. These aren’t theory pieces—they’re lived experiences. Whether you’re considering a switch, just did one, or are helping someone who is, this collection gives you the no-fluff facts you need to make smart choices.
Biosimilar switching lets patients move from expensive originator biologics to cheaper, equally effective versions. Learn what happens when you switch, why some people stop, and how to do it safely with proven data.
Read more