Osteodystrophy: what it is and why it matters
Osteodystrophy means abnormal bone growth or bone damage caused by another health problem. You’ll most often hear this term linked to chronic kidney disease (renal osteodystrophy), but other metabolic issues can cause it too. If you or someone you care for has long-term kidney problems, this is one of the bone issues clinicians watch for.
What causes osteodystrophy?
The common pathway is a disruption of mineral balance — mainly calcium, phosphate, and vitamin D — and changes in parathyroid hormone (PTH). Kidneys that don’t work well can’t activate vitamin D or remove phosphate properly. That imbalance forces the body to pull calcium from bones, making them weak, brittle, or misshapen. Other causes include hormonal problems and certain inherited or metabolic disorders.
Risk factors you can recognize include chronic kidney disease, long-term dialysis, low vitamin D, and some endocrine conditions. Certain medicines and prolonged immobilization also raise risk.
How osteodystrophy shows up
Symptoms vary. Some people notice bone pain, aching joints, or a bowed leg. Others find they break bones more easily or develop bone deformities over time. In kidney-related cases, you might also see muscle weakness, intense itching, or symptoms tied to low calcium like tingling or muscle cramps.
Not everyone has clear symptoms early on. That’s why testing is important if you have kidney disease or other risk factors.
Diagnosis: simple tests doctors use
Doctors start with blood tests: calcium, phosphate, PTH, alkaline phosphatase, and vitamin D levels. X-rays and bone density scans (DEXA) show bone loss or structural changes. In rare or unclear cases, a bone biopsy can give a definite answer about bone turnover.
Treatment and practical steps you can take
Treatment aims to correct the mineral imbalance and protect bone strength. That usually means managing phosphate (diet changes, phosphate binders), making sure you get the right form and dose of vitamin D, and treating high PTH levels if present. In some cases doctors use medications that alter bone turnover or recommend surgery for severe parathyroid problems.
Simple daily actions help too: follow a kidney-friendly diet if advised, avoid high-phosphate foods and cola drinks, stay active with weight-bearing exercise as tolerated, and protect yourself from falls. If you’re on dialysis, talk to your care team about mineral bone management — adjustments in dialysis, meds, or supplements can make a big difference.
If you notice new bone pain, fractures, or muscle cramps, see your doctor. Early changes are easier to manage than advanced bone damage.
Questions about medicines, supplements, or diet? Ask your nephrologist or pharmacist — they can tailor advice to your labs and overall health. Bone problems from other causes need a similar approach: find the root cause, correct lab abnormalities, and protect bone strength.
Osteodystrophy is manageable when caught early. Keep an eye on symptoms, get regular blood tests if you have kidney disease, and work with your care team on a clear plan to protect your bones.
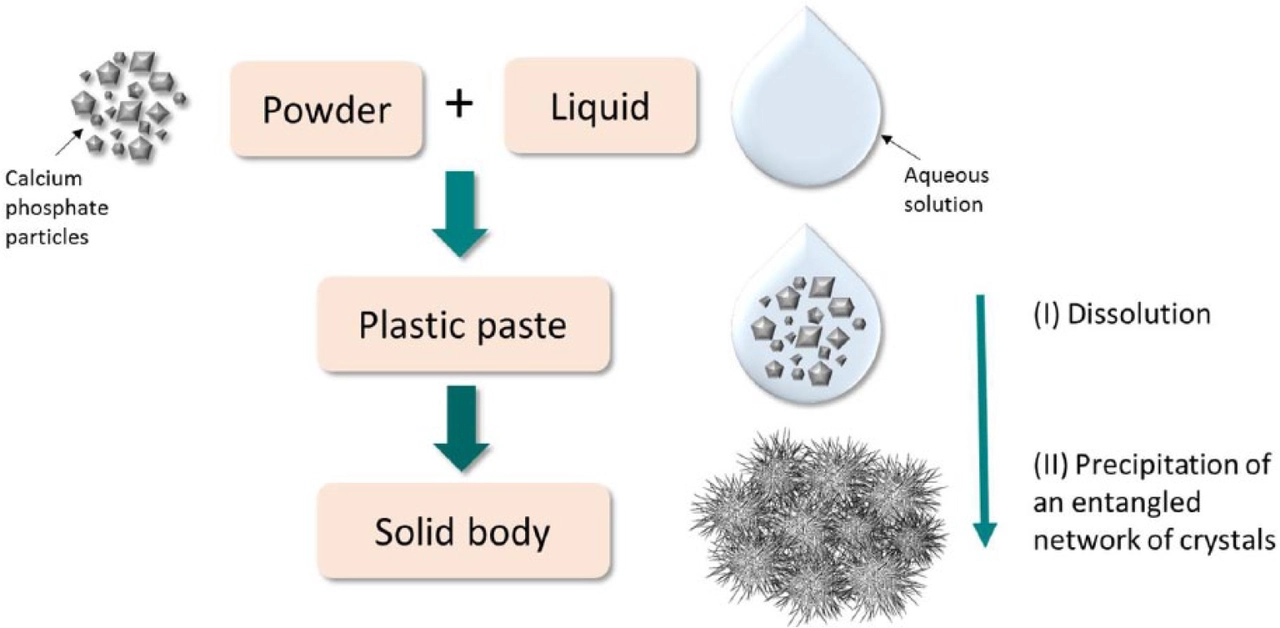
As a blogger, I've recently come across the importance of calcium and phosphorus in the development of osteodystrophy. These two minerals play a vital role in maintaining healthy bones and teeth. However, an imbalance in their levels can lead to osteodystrophy, a condition characterized by weak and deformed bones. To prevent this, it's essential to consume a balanced diet rich in calcium and phosphorus, and monitor their levels in the body. Additionally, it's crucial to consult a healthcare professional for guidance in managing these levels and maintaining overall bone health.
Read more