When you're on TRICARE, getting your prescriptions shouldn't feel like a maze. For most military families, generic drugs are the go-to choice-cheaper, just as effective, and covered under the program. But knowing TRICARE coverage for generics isn’t as simple as just saying "it’s generic." There are tiers, copays, formularies, and rules that change depending on where you fill your prescription and who you are.
How TRICARE Covers Generic Drugs
TRICARE doesn’t cover every generic drug just because it’s generic. It has a list-called the formulary-that tells you exactly which ones are covered. As of October 2025, TRICARE includes about 5,500 brand-name and generic medications on this list, with generics making up 92% of all prescriptions filled. That’s higher than most civilian insurance plans.
The key thing to understand: not every generic is automatically approved. Some generics are on the formulary, some aren’t. And even if a generic is on the list, you still have to pay something-unless you’re active duty.
The Four Tiers of TRICARE Drug Coverage
TRICARE organizes drugs into four tiers. For generics, it’s mostly Tier 1, but here’s how it all breaks down:
- Tier 1: Generic formulary drugs - These are the cheapest, most preferred options. Most common medications like lisinopril, metformin, or atorvastatin fall here.
- Tier 2: Brand-name formulary drugs - These are covered, but cost more. You’ll pay higher copays unless there’s no generic available.
- Tier 3: Non-formulary drugs - These aren’t on the approved list. You can still get them, but you need a medical necessity approval. About 15-20% of generic requests fall here.
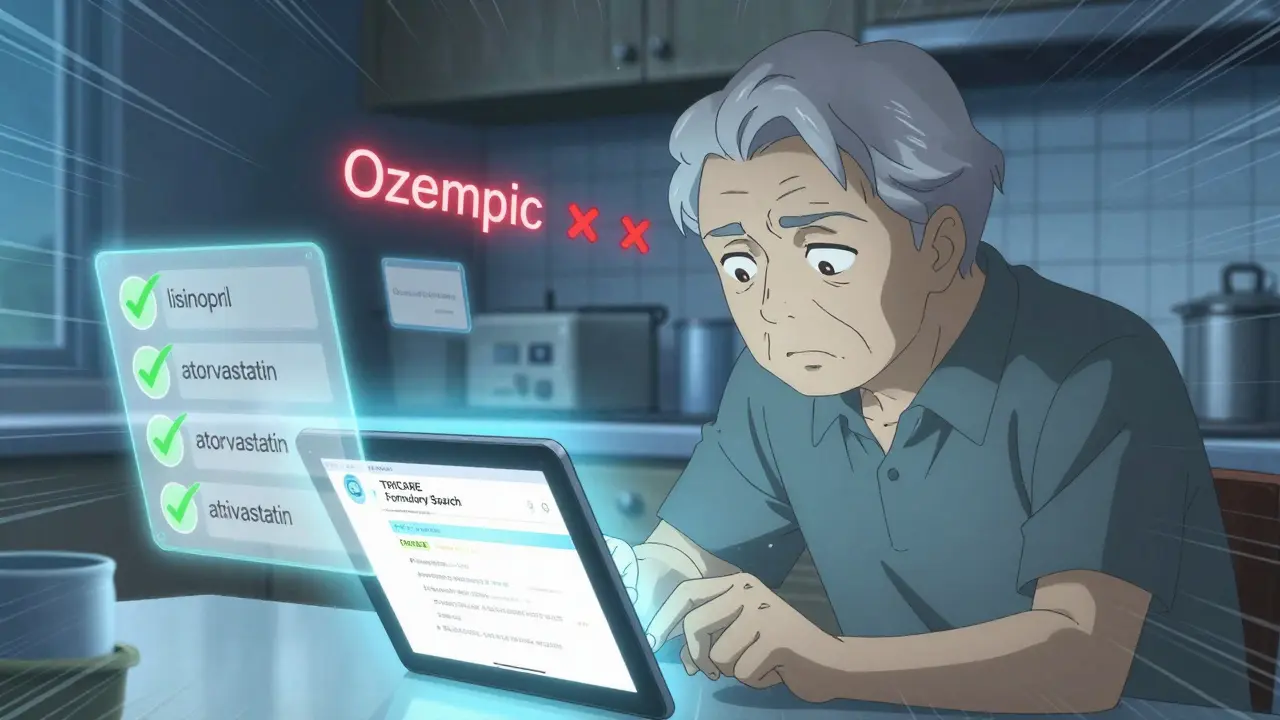
- Tier 4: Non-covered drugs - These aren’t covered at all. Examples include weight loss medications like semaglutide (Ozempic) and liraglutide (Saxenda), which were removed from coverage for TRICARE For Life beneficiaries as of August 31, 2025.
Where You Fill Your Prescription Changes the Cost
One of the biggest advantages of TRICARE is how much you save depending on where you get your meds. Here’s what you pay in 2025 for a Tier 1 generic:
| Pharmacy Type | 30-Day Supply | 90-Day Supply |
|---|---|---|
| Military Pharmacy | $0 | $0 |
| TRICARE Home Delivery (Express Scripts) | N/A | $13 |
| Network Retail Pharmacy | $16 | N/A |
Active duty service members pay nothing at any pharmacy. Retirees and family members pay the rates above. The big savings come from military pharmacies-if you live near one, use it. A 90-day supply of a generic cholesterol drug through home delivery costs $13. At a civilian pharmacy, you’d pay $30 or more.
How to Check If Your Generic Is Covered
You can’t assume a drug is covered just because it’s generic. The TRICARE Formulary Search tool (available at esrx.com/tform) is your best friend. Just type in the drug name and strength. It will tell you:
- Which tier it’s on
- What your copay will be
- Whether prior authorization is needed
Many users report confusion when their doctor prescribes a generic that’s not on the formulary. That’s because there are thousands of generic versions of the same drug-only some are approved by TRICARE. If your drug isn’t listed, you’ll need to request a medical necessity exception. About 78% of those requests get approved, but it can take up to 72 hours. That means you might have to delay your refill or make an extra trip to the clinic.
What’s Not Covered-and Why
Not all generics are treated equally. As of August 31, 2025, TRICARE stopped covering weight loss drugs like semaglutide and liraglutide for TRICARE For Life beneficiaries (mostly retirees over 65). This was a policy change tied to the 2024 National Defense Authorization Act. About 1.2 million people were affected.
Some other generics may be excluded because:
- They’re newer and haven’t been reviewed yet
- There’s a cheaper, equally effective alternative already on the formulary
- They’re considered non-essential (like some cosmetic or non-life-saving medications)
Biologic generics (like those for rheumatoid arthritis or Crohn’s disease) face even stricter rules. They require 22% more prior authorizations than regular generics because of complex FDA interchangeability rules.
How TRICARE Compares to Other Plans
TRICARE isn’t the cheapest for generics-but it’s not the worst. Medicare Part D averages $7-$10 for generics. TRICARE’s $13-$16 copays seem high, but here’s the catch: Medicare doesn’t have free military pharmacies. If you’re a retiree, TRICARE’s $0 copay at base pharmacies gives you a real edge.
Compared to the VA, TRICARE requires copays for most people. VA gives free meds to eligible veterans. But TRICARE covers more people-nearly 9.5 million-and offers broader access through retail and home delivery.
Most civilian employer plans have higher copays than TRICARE’s retail rate, but they often have wider formularies. TRICARE’s formulary is tighter. If your doctor prescribes something off-list, you’re stuck waiting for approval.
Real Stories from TRICARE Users
On Reddit, a Marine Corps retiree wrote: "My generic cholesterol pill costs $14 for 90 days through home delivery. My civilian friends pay $30 for 30 days. That’s a 70% savings." That’s the kind of win TRICARE delivers.
But others aren’t happy. A 68-year-old retiree on a forum said: "I’ve been on Ozempic for diabetes and weight loss. Now I’m paying $1,200 a month out of pocket. TRICARE dropped it, and Medicare won’t cover it either. I’m stuck."
Another common complaint: pharmacists at retail pharmacies don’t always know TRICARE rules. One user reported being charged $48 for a generic because the cashier didn’t know TRICARE had a network agreement. Always double-check your receipt. If you’re overcharged, call the TRICARE Pharmacy Helpline at 1-877-363-1303.

What’s Changing in 2026
On January 1, 2026, TRICARE’s home delivery copay for generics will go from $13 to $14. Retail stays at $16. Military pharmacies remain $0.
TRICARE is also rolling out new tools:
- Real-time benefit checks by Q3 2026-your doctor will see your copay and coverage before they write the script.
- Step therapy expansion to 15 more drug classes by 2027-you might need to try a cheaper generic first before getting a more expensive one.
- Pharmacogenomic testing by 2028-some high-risk meds will require genetic testing to ensure they’re safe for you.
These changes aim to cut waste and improve safety. But they also mean more paperwork and delays for some users.
How to Use TRICARE Generics the Smart Way
Here’s how to avoid headaches:
- Always check the TRICARE Formulary Search tool before your doctor writes a script.
- Use military pharmacies whenever possible-$0 is $0.
- For chronic conditions (like high blood pressure or diabetes), sign up for TRICARE Home Delivery. It’s cheaper and you get 90-day supplies.
- If your generic isn’t covered, ask your doctor to request a medical necessity exception. Have your medical records ready.
- Keep a list of your medications and their formulary status. Update it every time you get a new prescription.
Most people using TRICARE for generics report high satisfaction-86% in the 2025 beneficiary survey. The biggest complaints come from those who need non-formulary drugs or were hit by the weight loss medication cutoff.
Final Takeaway
TRICARE coverage for generics is one of the program’s strongest features. It saves beneficiaries billions every year and keeps medications accessible. But it’s not perfect. You need to be proactive. Know your tier. Know your pharmacy. Know your formulary. And if something doesn’t look right, call TRICARE. Don’t assume. Don’t wait. A $14 copay today can turn into a $1,200 bill tomorrow if you don’t check.
Are all generic drugs covered by TRICARE?
No. TRICARE only covers generics that are on its formulary. Even if a drug is generic, it may be excluded if there’s a cheaper alternative, it’s not FDA-approved for your condition, or it’s been removed due to policy changes (like weight loss drugs as of August 2025). Always check the TRICARE Formulary Search tool before filling a prescription.
Why is my generic drug not covered even though it’s the same as the brand name?
TRICARE doesn’t cover every version of a generic drug. Different manufacturers make generics, and TRICARE only approves specific ones based on cost, availability, and clinical equivalence. Your doctor may have prescribed a generic from a manufacturer that’s not on the formulary. You can request a medical necessity exception, or ask your doctor to switch to a covered version.
Can I get my generic prescription filled at any pharmacy?
You can fill at any pharmacy, but your cost changes. Military pharmacies cost $0. Network retail pharmacies charge $16 for a 30-day supply. Non-network pharmacies may charge more and require you to pay upfront and file for reimbursement. Always use a TRICARE network pharmacy to avoid surprise bills.
What’s the difference between TRICARE Home Delivery and retail pharmacies?
Home Delivery (through Express Scripts) gives you 90-day supplies for $13 in 2025, ideal for chronic conditions. Retail pharmacies fill 30-day prescriptions on the spot for $16. Home Delivery is cheaper long-term, but takes 7-10 days to process. Retail is faster but more expensive per day. Active duty members get both for free.
Why did TRICARE stop covering weight loss generics?
As of August 31, 2025, TRICARE For Life beneficiaries (retirees and their spouses over 65) lost coverage for weight loss medications like semaglutide and liraglutide. This change was mandated by the 2024 National Defense Authorization Act. The program still covers these drugs for active duty and younger beneficiaries if prescribed for diabetes or other covered conditions.
How do I request a prior authorization for a non-formulary generic?
Your doctor must submit a medical necessity request through the TRICARE provider portal. You’ll need documentation showing why the formulary generic won’t work for you. Approval usually takes 48 hours, but can take up to 72. You can call the TRICARE Pharmacy Helpline at 1-877-363-1303 for help tracking your request.
Will TRICARE’s generic copays keep going up?
Copays have increased slowly over time. The $13 to $14 increase for home delivery in 2026 is the first change since 2023. Experts predict minimal impact on adherence because the $0 military pharmacy option remains. Future increases will likely be tied to inflation and federal budget decisions, but TRICARE aims to keep generics affordable to encourage use.








Comments
Let me guess - you think TRICARE’s formulary is some kind of benevolent gift from the gods? Nah. It’s a cost-cutting algorithm disguised as healthcare. They don’t care if your generic works - they care if it’s the cheapest version made by the manufacturer who paid the best kickback. I’ve had my blood pressure med switched three times because some corporate bean counter decided a different batch was ‘equivalent.’ It’s not. My body knows the difference. And now I’m stuck waiting 72 hours for a prior auth just to get back to the drug that didn’t give me headaches. This isn’t coverage. It’s a lottery with extra steps.
If you're on TRICARE and not using military pharmacies, you're leaving money on the table. Period. I refill my 90-day supply of metformin through home delivery for $13 - my neighbor pays $47 at CVS for the same thing. Stop overcomplicating it. Use the formulary tool. Know your tiers. Don’t let your pharmacist guess your coverage. And if you’re retired and living near a base? Walk in. Get it for free. It’s not magic. It’s just basic math.
The real tragedy isn’t the copays. It’s the illusion of choice. We’re told generics are interchangeable. But the system tells us no - not all generics are created equal. Only the ones the bureaucracy deems acceptable. It’s not medicine. It’s rationing dressed in clinical language. We’re not patients. We’re data points in a spreadsheet that prioritizes budget over biology. And yet we’re supposed to be grateful because $13 is better than $30. That’s not progress. That’s surrender.
I’m curious - when TRICARE says a generic isn’t covered because there’s a cheaper alternative, how do they define ‘equally effective’? Is it based on clinical trials? Real-world outcomes? Or just price per pill? I’ve seen doctors switch me to a different generic because it was ‘preferred,’ but my bloodwork didn’t improve. I had to fight for three weeks to get back to the original. I wish there was more transparency around how these decisions are made.
Y’all need to chill 😌 TRICARE generics are still way better than most private insurance. My mom’s Medicare Part D copay for her statin is $22. I pay $13 for the same thing through home delivery. And if you live near a base? FREE. That’s not a bug - it’s a feature. Yes, the formulary is tight. But 92% of prescriptions are covered. That’s insane compared to civilian plans. Use the tool. Call the helpline. Don’t assume. But also - don’t turn a solid benefit into a victim narrative. You’re lucky. Really.
It’s evident that the current formulary architecture reflects a sophisticated pharmacoeconomic framework optimized for marginal cost efficiency while maintaining therapeutic equivalence thresholds as defined by the TRICARE Formulary Review Committee under DHA Directive 2023-017. The exclusion of non-interchangeable biologics aligns with CMS guidelines and the FDA’s 2024 biosimilar interchangeability criteria. That said, the absence of real-time formulary integration at point-of-prescribing remains a systemic friction point - a suboptimal user experience in an otherwise high-efficiency ecosystem.
For anyone feeling overwhelmed by the formulary or prior auth process - you’re not alone. I used to stress every time I needed a refill. Then I started keeping a simple spreadsheet: drug name, tier, copay, pharmacy I used, and whether it was approved. I share it with my pharmacist now - they actually appreciate it. And if you’re stuck? Call TRICARE. They’re not perfect, but they’ll help. This system isn’t designed for convenience - it’s designed for sustainability. But you can still make it work for you. Small steps. One script at a time.
People who complain about the $14 home delivery copay are the same ones who think Ozempic should be free. You don’t get to demand expensive drugs and then cry when the military stops paying for your weight loss pills. TRICARE isn’t your personal pharmacy. It’s a defense benefit. If you need $1,200/month drugs, maybe don’t retire at 65 and expect the government to foot the bill. Stop acting like a victim. You signed up for this.