Drug Competition: How Generic, Biosimilar, and Brand Drugs Fight for Your Prescription
When you hear drug competition, the market battle between brand-name, generic, and biosimilar medications that drives down prices and increases access. Also known as pharmaceutical market competition, it’s not just about corporate profits—it directly affects how much you pay, what options your doctor offers, and even how safe your treatment is. This isn’t theoretical. Every time you pick up a cheaper pill labeled "generic," you’re seeing drug competition in action. But it’s more than just price tags. It’s about whether a biosimilar can safely replace an expensive biologic like Humira, whether your insurance pushes you toward a generic statin, or why your pharmacist asks if you mind switching brands.
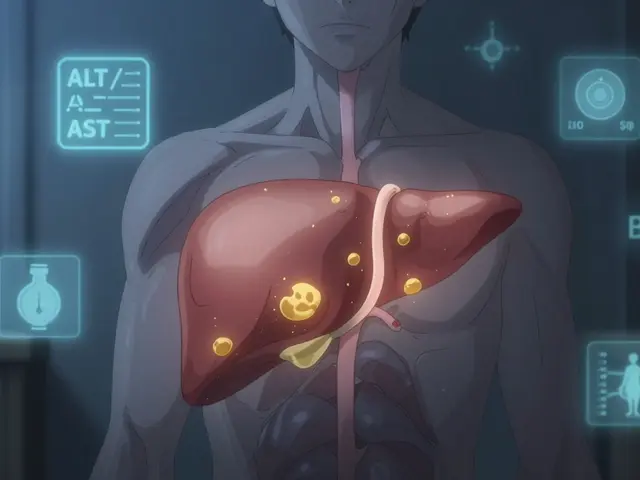
Drug competition isn’t just between companies—it’s between generic medications, chemically identical versions of brand-name drugs that enter the market after patents expire. Also known as non-brand drugs, they make up over 90% of prescriptions in the U.S. because they cost up to 85% less. Then there’s biosimilar switching, the process of moving from a costly originator biologic to a highly similar, lower-cost version like an adalimumab biosimilar. Also known as biologic substitution, it’s changing how chronic conditions like rheumatoid arthritis and Crohn’s are managed—especially when patients are told to switch to save money. And let’s not forget brand name drugs, the original, patented medications developed by pharmaceutical companies and marketed under proprietary names like Deltasone or Cialis. Also known as innovator drugs, they’re the ones with big ad budgets, but also the ones that set the high prices everyone else tries to beat. These three types are locked in a constant tug-of-war. When a biosimilar enters the market, the brand-name drug’s price often drops. When a generic hits, pharmacies start favoring it. And when insurers create tiered formularies, they’re basically forcing drug competition to work in their favor—and yours.
What you’ll find in this collection isn’t just theory. It’s real stories: how people switched from Humira to a biosimilar and saved thousands, why grapefruit juice can break the rules of drug competition by making generics dangerously potent, how vegans navigate hidden animal ingredients in pills, and why a boxed warning on a drug might make a cheaper alternative the smarter choice. You’ll see how medication safety, insurance rules, and patient trust all tie into who wins and who loses in this hidden battle. Whether you’re paying out of pocket, dealing with insurance denials, or just wondering why your pill looks different this month—this is the system behind it. The next time you get a prescription, you’ll know exactly what’s really being fought over.
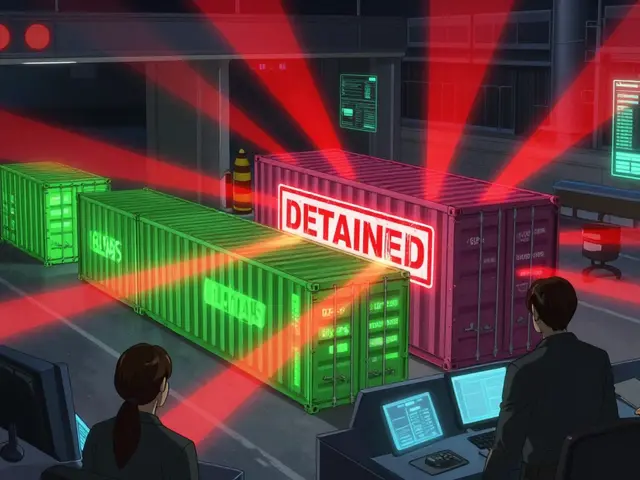
Biologic drugs in the U.S. enjoy 12 years of exclusivity before biosimilars can enter. Complex patents, high development costs, and legal delays keep prices high. Here’s how the system works-and why patients pay more than in Europe.
Read more