Digestive Health: Practical Tips and Treatment Options
Stomach pain, bloating, constipation or frequent heartburn — these are signals your digestive system needs attention. I’ll give clear steps you can try today to feel better and when to see a doctor. No fluff, just useful actions.
Simple diet and lifestyle fixes
Start with water: drink regularly and aim for about 8 glasses a day unless your doctor says otherwise. Fiber helps; add fruits, vegetables, whole grains, and beans slowly to avoid gas. If you get bloated, try low-FODMAP choices like bananas, carrots, oats, and rice for a while to test triggers. Eat smaller meals more often and chew slowly — that can cut reflux and bloating.
Move daily. A 20–30 minute walk after meals speeds digestion and reduces constipation. Cut down on alcohol, sugary drinks, and fried foods; they commonly worsen heartburn and loose stools. Smoking makes reflux worse, so quitting helps your gut as well as your lungs.
When supplements and medicines help
Probiotics can reduce some diarrhea and bloating for certain people. Try a multi-strain probiotic for four weeks and note any improvement. Fiber supplements like psyllium work if you struggle to eat enough fiber, but add them gradually with water to avoid cramps. Over-the-counter antacids or acid reducers can ease heartburn for short periods; persistent symptoms deserve medical review.
For long-term or severe conditions like ulcerative colitis, medication and specialist care are usually needed. If you’re curious about natural approaches for ulcerative colitis, read our article "Natural Remedies for Ulcerative Colitis: Do They Work?" where we weigh diet, herbs, and lifestyle against research and safety concerns.
Watch for warning signs: unintentional weight loss, blood in stool, persistent vomiting, high fever, or severe abdominal pain. Those need immediate evaluation. Also get checked if symptoms interfere with daily life or don’t improve after basic changes.
Track what you eat and how you feel. A simple food-and-symptom diary for two weeks often reveals patterns faster than guessing. When you try a change, test one variable at a time — for example, swap coffee for tea for a week — so you can tell what helped.
Tests that help pinpoint causes include blood work, stool tests for infection or inflammation, breath tests for lactose or SIBO, and scopes or imaging when bleeding or persistent inflammation is suspected. Testing removes guesswork and guides treatment. If inflammation is found, medicine differs from care for functional issues like IBS.
Stress and sleep matter. Poor sleep or chronic stress can worsen pain, motility, and inflammation. Try simple breathing, 10 minutes of relaxation, and a regular sleep schedule before blaming food. Also check medicines — common drugs like NSAIDs, antibiotics, or some supplements can upset the gut. Talk over your full list of meds with your clinician to rule out drug-related causes.
Small steps add up fast. Stick with them daily.
Use trusted sources and ask questions: your primary care doctor, a gastroenterologist, or a registered dietitian can give clear, targeted advice. Quick fixes can help symptoms, but a clear plan based on your diagnosis leads to steady improvement.
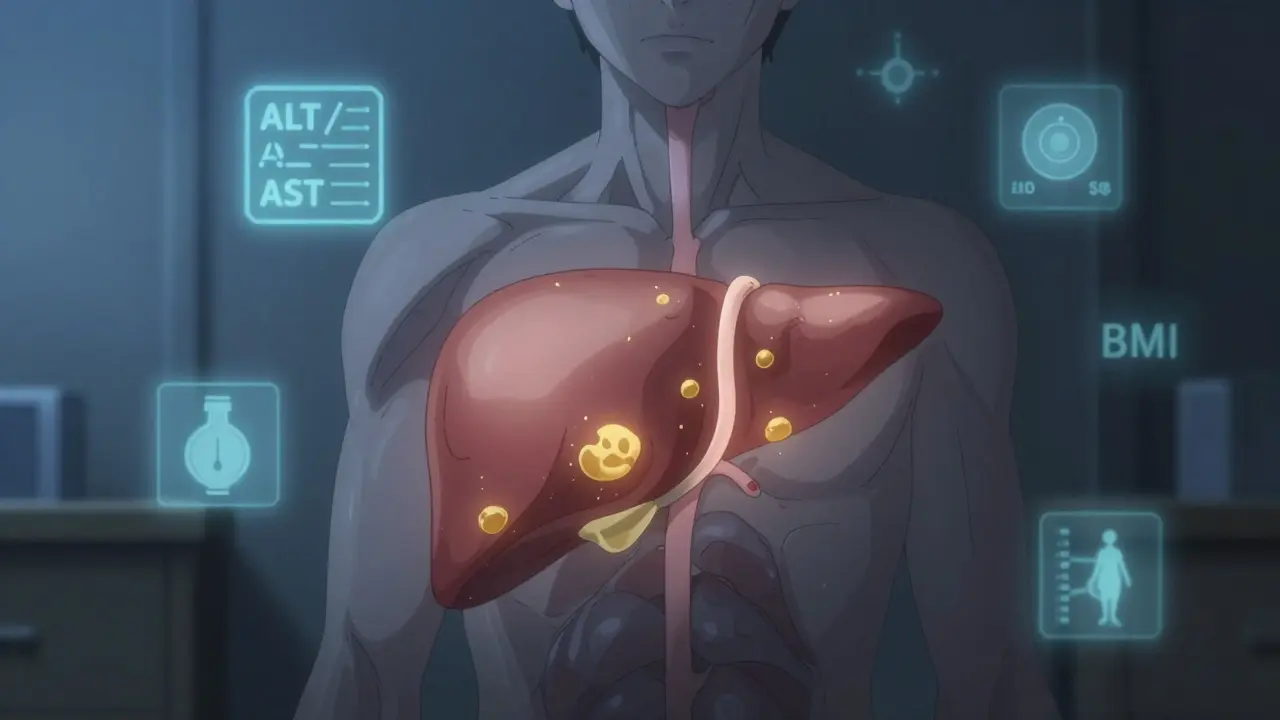
Understand the key differences between NAFLD and NASH, how fibrosis develops, and what steps you can take to prevent liver damage. Learn about symptoms, risk factors, and the latest updates in fatty liver disease.
Read more
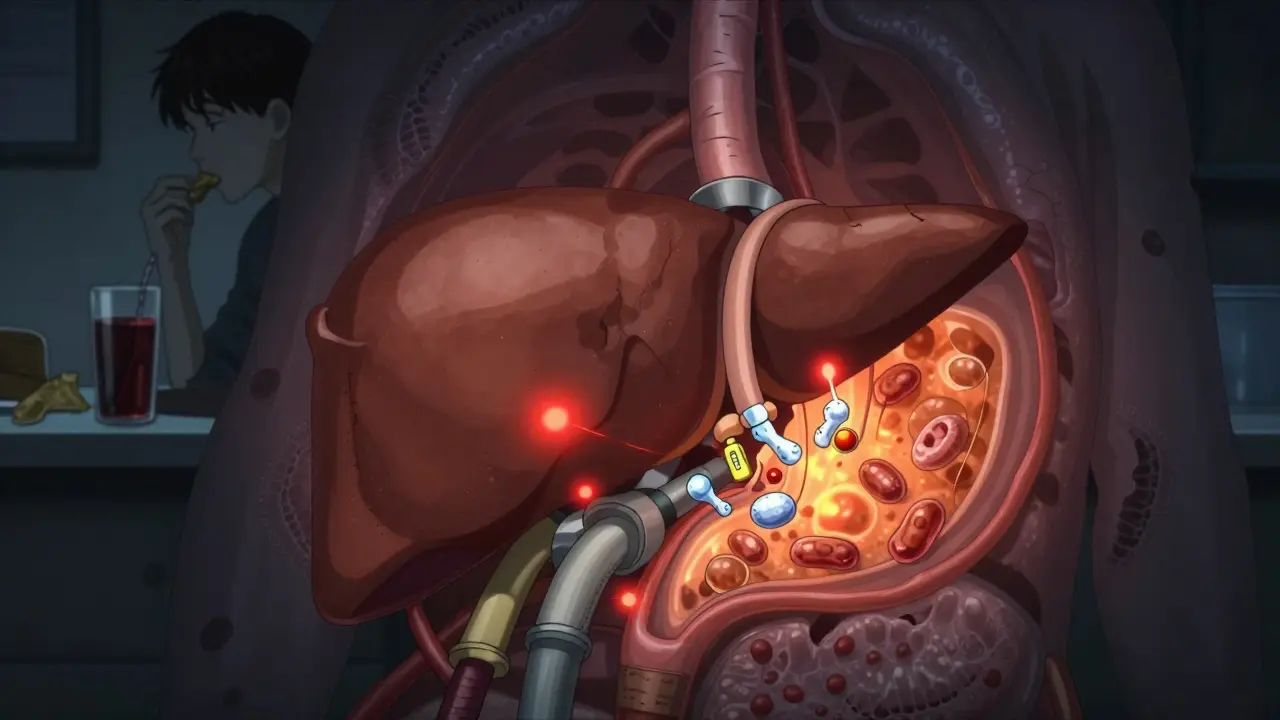
Gastroparesis causes delayed stomach emptying, leading to nausea, bloating, and early fullness. Learn how diet changes - small meals, low fat, blended foods - can reduce symptoms and improve quality of life for most patients.
Read more
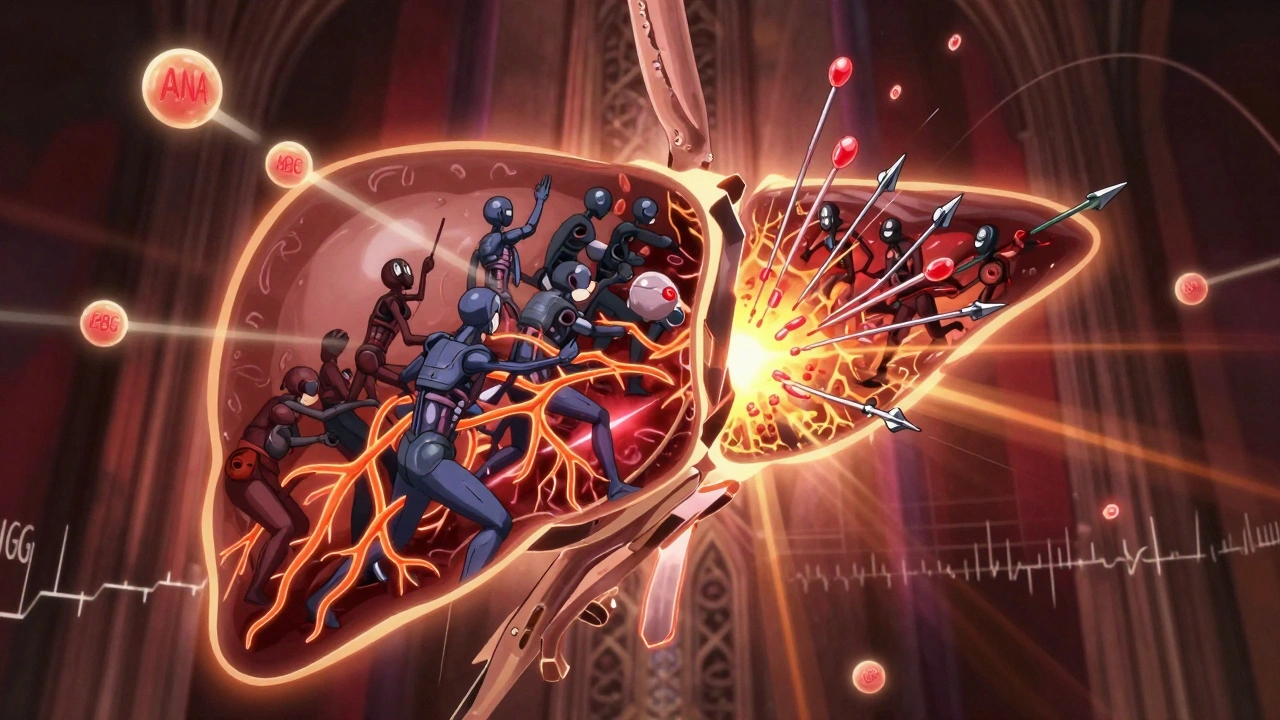
Autoimmune overlap syndromes like AIH-PBC combine features of multiple liver diseases, requiring careful diagnosis and dual treatment. Learn how PBC, PSC, and AIH interact-and why missing an overlap can lead to faster liver damage.
Read more
Diverticulitis is inflamed pouches in the colon that cause severe abdominal pain and fever. Learn the real causes, modern treatments, and proven ways to prevent recurrence-without outdated myths about nuts and seeds.
Read more
Ulcerative colitis, a chronic ailment affecting the colon, often prompts individuals to explore natural remedies in search of symptom relief. This article dives into the practicality of these natural treatments, evaluating how lifestyle alterations, dietary adjustments, and herbal supplements can potentially ease the condition. While some individuals report anecdotal benefits, it's crucial to balance optimism with scientific understanding. We explore popular natural methods and their plausible impacts on the gut lining, aiming to separate fact from hopeful fiction.
Read more