Every year, over 1.3 million medication errors happen in the U.S. - not because people are careless, but because they simply don’t understand what the label says. You might think you know how to read a prescription: ‘Take one tablet twice daily.’ But what does that really mean? Morning and night? After breakfast and dinner? Or just any two times 12 hours apart? If you’re unsure, you’re not alone. Nearly half of all adults struggle to make sense of basic medication instructions.
Why Medication Labels Are So Confusing
Most prescription labels were designed by pharmacists for pharmacists. They use terms like ‘q12h,’ ‘PO,’ or ‘as needed,’ which mean nothing to most people. A 2009 study found that 47% of patients misinterpreted standard instructions like ‘Take 1 tablet by mouth twice daily.’ Even when rewritten in plain language - ‘Take 1 tablet in the morning and 1 tablet in the evening’ - comprehension only improved by 15-20%. That’s still a big gap.It’s worse for older adults, people with low literacy, or those juggling five or more medications. One patient told researchers she thought ‘take every 4-6 hours’ meant she could take 4 to 6 pills at once. Another confused ‘mg’ (milligrams) with ‘ml’ (milliliters) and overdosed on liquid medicine. These aren’t mistakes from carelessness - they’re mistakes from unclear communication.
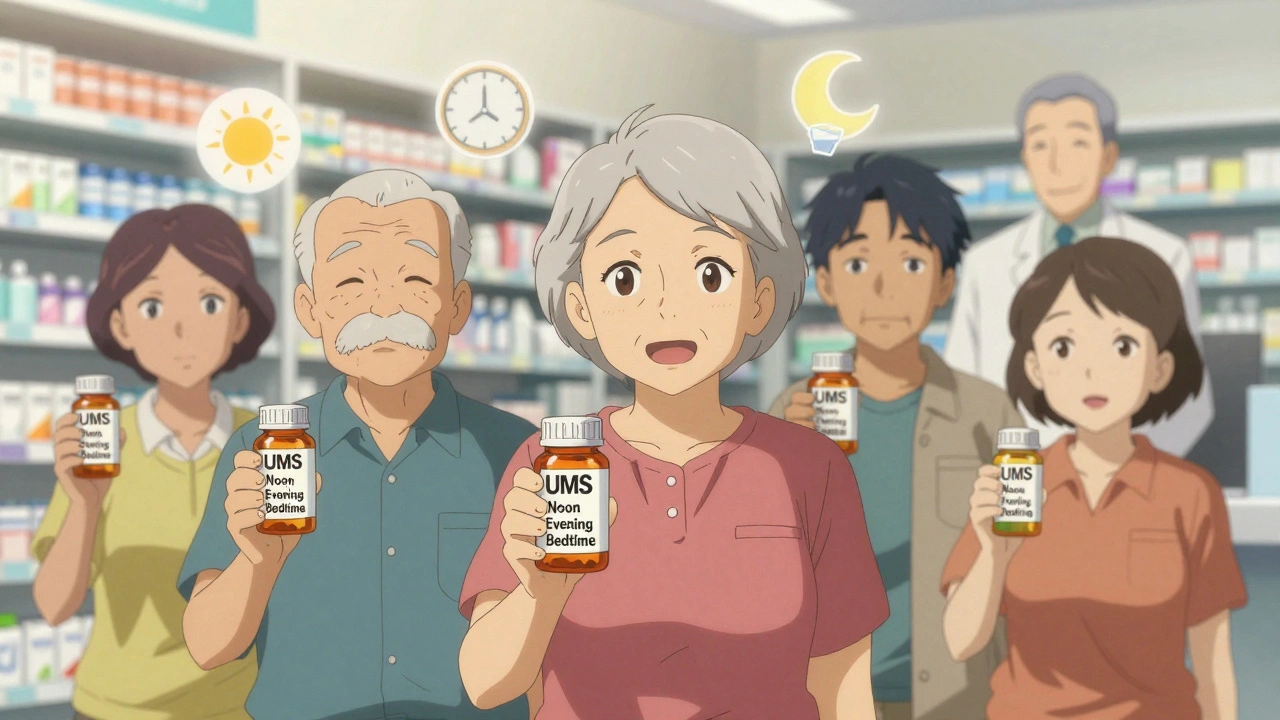
The Universal Medication Schedule (UMS): A Simple Fix
One of the most effective tools to fix this is the Universal Medication Schedule (UMS). Instead of saying ‘twice daily’ or ‘q8h,’ UMS uses four clear times: morning, noon, evening, bedtime. No math. No guesswork. Just four times you can remember.When UW Health in Wisconsin switched to UMS labels, dosing confusion dropped by 47% among elderly patients. One 72-year-old woman with diabetes, high blood pressure, and arthritis said: ‘I finally understood when to take my pills.’ Before, she was mixing up her meds. After? She took them correctly every day.
UMS works because it matches how people actually live. Most of us don’t think in ‘every 8 hours.’ We think in meals and routines: breakfast, lunch, dinner, and before bed. That’s why UMS is now used in over 68% of large U.S. health systems - and it’s required under new U.S. Pharmacopeia (USP) guidelines that took full effect in May 2025.
Pictograms: Pictures That Save Lives
Words aren’t enough. That’s why pictograms - simple pictures that show how to take medicine - are becoming standard. A picture of a person drinking water with a pill. A clock showing morning and night. A hand holding a cup with a drop of liquid.Studies show pictograms improve understanding by 28% for people with low health literacy. In pediatric settings, where parents are often stressed and sleep-deprived, pictograms cut dosing errors in half. One 2012 review found that 63% of children’s liquid medicine labels used confusing charts like ‘5 mL for 20-25 lbs.’ But when they switched to a picture of a syringe with a line at 5 mL, parents got it right 92% of the time.
By 2024, the FDA plans to require standardized pictograms on all prescription labels. This isn’t just nice to have - it’s becoming the law. And for good reason: a patient once drank albuterol from a plastic container because the label didn’t show it was meant to be inhaled, not swallowed. That’s the kind of mistake pictograms can prevent.

Teach-Back: The Most Powerful Tool You’re Not Using
Even the clearest label won’t help if you don’t understand it. That’s where teach-back comes in. It’s simple: after the pharmacist or nurse explains your medicine, they ask you to explain it back in your own words.‘Can you tell me how you’ll take this pill?’
‘So you’ll take one in the morning and one at night, right?’
This takes just 1-2 minutes per medication - but it cuts misunderstanding rates by 33%. At Children’s Hospital of Philadelphia, a 2023 trial found that caregivers who went through teach-back made 34% fewer dosing errors with liquid medicines. One mother thought ‘5 mL twice daily’ meant 5 mL total - not 5 mL each time. Teach-back caught it before she gave the wrong dose.
It’s not about testing you. It’s about making sure you’re safe. And if you can’t explain it? That’s not your fault. It’s the system’s job to make it clear.
What You Can Do Right Now
You don’t have to wait for the system to fix itself. Here’s what you can do today:- Ask for UMS labeling. If your pharmacy still uses ‘twice daily,’ ask if they can change it to ‘morning and evening.’ Most will.
- Use a pill organizer. Fill it with the times you know: morning, noon, evening, bedtime. It’s a visual backup.
- Take a picture of your label. Save it on your phone. Zoom in. Read it out loud. Does it make sense?
- Ask: ‘What happens if I miss a dose?’ This reveals hidden instructions.
- Use the teach-back method yourself. After a pharmacist explains something, say: ‘Just to make sure I got it - you want me to take one in the morning and one at night, right?’

Why This Matters More Than You Think
Medication errors aren’t just about taking too much or too little. They lead to hospital visits, falls, kidney damage, and even death. The CDC says people with low health literacy are 2.5 times more likely to misinterpret dosing instructions. That’s not a small risk - it’s a public health crisis.But here’s the good news: we know how to fix it. Simple labels. Clear pictures. Plain language. Teach-back. These aren’t fancy tech solutions. They’re basic human communication. And when done right, they work.
Every $1 spent on health literacy tools saves $3.75 in hospital costs. That’s why hospitals are adopting these strategies - not just for safety, but because Medicare penalizes them for preventable readmissions.
It’s not about being smart or dumb. It’s about clear communication. And you deserve to understand your medicine - no matter your education level, age, or background.
What’s Coming Next
By 2025, all U.S. prescription labels must follow USP <17> standards: fifth-grade reading level, one-column layout, no jargon, pictograms, and standardized timing. Merck is developing an AI tool to test label comprehension before printing. The CDC is rolling out a national test to measure how well people understand labels.But change doesn’t happen overnight. Small pharmacies still use outdated labels. Rural clinics lack training. Some doctors still say ‘take it as needed’ without explaining what that means.
That’s why your voice matters. If you don’t understand a label - say so. Ask for help. Ask for pictures. Ask for it in plain language. You’re not being difficult. You’re being smart.
What does ‘take twice daily’ really mean?
‘Take twice daily’ is vague. It could mean every 12 hours, or just morning and night. The safest approach is to ask for the Universal Medication Schedule (UMS): ‘Take one in the morning and one in the evening.’ If you’re unsure, check with your pharmacist - don’t guess.
Can I trust the dosage on over-the-counter medicine labels?
Not always. A 2012 study found that 18.5% of top-selling children’s liquid medicines didn’t list active ingredients on the front. Many used confusing charts instead of clear measurements. Always look for ‘mL’ or ‘tsp’ and use the dosing tool that comes with it - never a kitchen spoon. If in doubt, call your pharmacist.
Why do some labels say ‘take with food’ and others say ‘take after meals’?
There’s no standard. ‘With food’ could mean during, before, or after. The FDA is working on fixing this, but for now, ask your pharmacist: ‘Should I take this right before eating, during, or after?’ Write it down. This inconsistency causes many errors.
Is it safe to split pills if the dose is too high?
Only if the pill is scored (has a line down the middle) and your doctor or pharmacist says it’s okay. Some pills are designed to release medicine slowly - splitting them can make you sick. Never split capsules or tablets labeled ‘extended-release’ or ‘SR.’
What should I do if I think I took too much?
Call your pharmacist or poison control immediately - don’t wait for symptoms. Keep the medicine bottle handy so you can tell them the exact name, dose, and time you took it. Many errors are caught before they cause harm when people act fast.
Are there apps that help me understand my meds?
Yes. Apps like MyTherapy, Medisafe, and PillPack let you scan your label and set reminders with plain-language alerts. Some even show pictograms and explain side effects in simple terms. But they’re not a replacement for asking questions - use them as a helper, not a final answer.
Final Thought: You’re Not Alone
You’re not lazy. You’re not confused because you’re not smart. You’re confused because the system wasn’t built for you. But things are changing. Labels are getting clearer. Pictures are becoming standard. Pharmacists are being trained to ask, not assume.And you? You have the power to ask for better. To say, ‘I need this in plain words.’ To use a pill organizer. To take a picture of your label. To teach-back what you hear.
Medication safety isn’t just a hospital policy. It’s a human right. And you deserve to take your medicine without fear - because you know exactly what it is, when to take it, and why it matters.






Comments
This is literally life-saving info 🙌 I used to mix up my grandma's meds until I saw the UMS labels at her pharmacy. Now she takes everything on time. Why isn't this standard everywhere??
The teach-back method is the most underused tool in healthcare. I work in a clinic and we started implementing it six months ago. Adherence rates jumped 40%. It’s not about testing patients-it’s about validating understanding. Simple. Effective. Human.
This is all just government overreach... next they'll tell us how to breathe! Why can't people just READ?!?!!? I mean, come ON. It's not rocket science!
I’ve been a pharmacist in rural Maine for 22 years. The UMS change? Game-changer. Before, we’d spend 10-15 minutes per patient explaining ‘q12h’ or ‘as needed.’ Now? We say ‘morning and bedtime.’ They nod. They get it. No more frantic calls at 2 a.m. because someone took six pills thinking ‘every 4-6 hours’ meant a range. It’s not fancy tech. It’s just speaking like a person.
Honestly, the entire pharmaceutical-industrial complex is a linguistic minefield designed to obfuscate. The term ‘as needed’ is a neoliberal trap-a performative illusion of autonomy that actually shifts responsibility onto the most vulnerable. Pictograms are merely performative decolonization of the pharmacopeia. We need epistemic justice, not emoji.
i love how this post breaks it down so simply. i used to think i was dumb because i kept mixing up my blood pressure meds... turns out the labels were just written like a legal contract. now i use my phone to snap pics and read em out loud. game changer. thanks for not talking down to us.
Ah yes, the UMS. The beautiful, elegant solution that somehow still requires a PhD in pharmacology to navigate the 37 different pill organizers on Amazon. Let’s not pretend this isn’t just another corporate rebranding of ‘just ask your pharmacist’ with a pretty picture. Still, I’ll take it over ‘q8h’ any day. 🤓
I’ve seen this in action with my dad. He’s 78, on 7 meds, barely reads. We switched to UMS labels and added color-coded pill boxes. He hasn’t missed a dose in 8 months. The real win? He stopped saying ‘I’m too old for this’ and started saying ‘I got this.’ That’s dignity. That’s what matters.
It’s fascinating how language constructs power in medical contexts. The use of Latin abbreviations like ‘q.d.’ or ‘p.o.’ is not merely archaic-it’s a mechanism of epistemic exclusion. The UMS doesn’t solve the hierarchy; it merely redistributes the burden of translation onto the patient’s cognitive labor. Still, I concede it’s a pragmatic step in a broken system. But what of the patients who lack caregivers to interpret pictograms? Or those whose first language isn’t English? The system still fails them.
Let’s be real-this whole ‘plain language’ movement is just a Band-Aid on a hemorrhaging system. Pharmacies are understaffed, doctors are overworked, and patients are treated like data points. You can give me a pictogram of a cup and a pill, but if the pharmacist is rushing me because they’ve got 12 more patients waiting, it doesn’t matter how ‘clear’ the label is. This isn’t about communication-it’s about resource allocation. And we’re not fixing that.
I’m from a small village in Mississippi. We don’t have a pharmacy with UMS labels. My cousin’s kid got sick because they used a teaspoon for liquid medicine. No one knew it was 5mL, not 5 tsp. We need community health workers. Not apps. Not pictures. People who come to your door.
I can’t believe people still think this is acceptable. My aunt died because she took too much Tylenol. The label said ‘every 6 hours’ and she thought that meant 6 pills. SIX PILLS. And now we’re just talking about PICTOGRAMS like that’s enough? This is a national tragedy and we’re treating it like a UX redesign.
America’s healthcare system is a joke. We spend billions on fancy apps and pictograms but still let pharmacies print labels in 6-point font. Meanwhile, in Germany, they print everything in bold, big letters with icons. Why? Because they care. Here? We care about profit. End of story.
The UMS is brilliant, but the real bottleneck is the EHR systems. Most pharmacy software still auto-generates labels using legacy templates. Until we force EHR vendors to adopt USP 2025 standards, this is all just lip service. I work in health IT-we’ve got the tech. We just need the mandate.
just wanted to say thanks to the person who wrote this. i printed it out and showed it to my mom. she cried. said she finally felt seen. that’s more than any app or pictogram can do.